NB: This blog originally appeared in Huffington Post Canada on Nov 3, 2015. With the demise of HuffPo it’s being reposted here for future reference.
As someone who had his formative years in the 1980s I can still vividly recall former First Lady Nancy Regan launching the ambitious “Just Say No” campaign. She championed this slogan as part of the “war on drugs.” This “war” was started by Richard Nixon in 1971. He declared that drug abuse was “public enemy number one” and that “the only way to fight this menace was on many fronts.” I can personally attest to having been a true believer in that policy myself, after having done some volunteer work in an emergency department as a teenager.
In recent years Canada of course, for the most part followed this policy. In our country, the main technique to fight this war appears to be conviction and incarceration of those caught with illicit drugs. For example, possession (not sale, but possession) is punishable by up to five years in prison. However, what’s clear is that this has failed to help the problem. Data from Statistics Canada (the most recent I could find) shows that while marijuana use in Canada has been relatively constant, the rate of cocaine and other drug use has gradually been increasing since 1977.
The drug trade itself has seemed to grow and is now considered to have a global value of over $300 billion (U.S.) per year. In Canada, as you can see below on this chart from Statistics Canada, drug offences continue to rise, while the total crime rate decreases. So certainly based on this data, it would be difficult to suggest that the “war” has been successful.
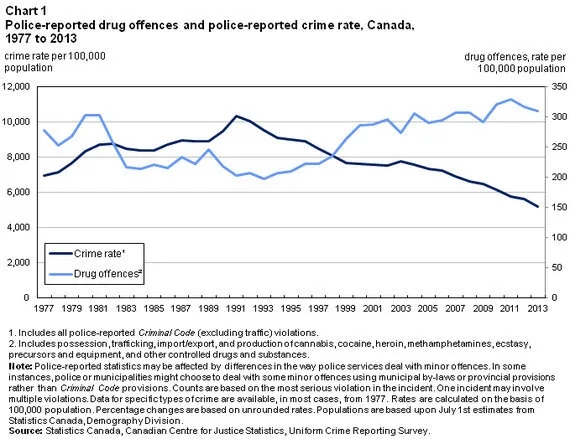
From an economic point of view, the costs of this war are even more staggering. It currently costs $117,000 a year to house a prisoner. Additionally, while the total overall rate of crime has decreased in the past twenty years, the incarceration rate is up, and 80 per cent of offenders have substance abuse problems. It’s clearly not hard to postulate that the main reason for the increased rate of incarceration is drug offences.
As a family physician, I have seen first hand the effects of untreated drug addiction. Far beyond the relatively easy to measure economic numbers, lives have been ruined, families torn apart, some young women forced into the sex trade to pay for their habit and more, are all part and parcel of this terrible disease. Clearly, the goal of any national policy should be to take proven effective steps to reduce the rate of addiction.
The newly elected Liberal government of Justin Trudeau plans to legalize marijuana. To that end, my hope is that Canada can go one step further and focus on what works to reduce addiction rates. While it is clearly counter intuitive to suggest this, it turns out that the best way to do this, is to decriminalize the possession of small amounts of drugs.
While about 25 countries have decriminalized drugs, the best example of how this policy works is seen in Portugal. They decriminalized the possession (not sale, possession) of drugs for personal use in 2001. The offence was re-classified to an administrative offence as opposed to a criminal one, punishable at most by a fine. At the time, may people, myself included I might add, predicted that this would lead to an explosion of drug use, and that children would be targeted, and the nation would decay. As an aside, this rhetoric is similar to what Stephen Harper alleged would happen if we were to legalize marijuana in the last election. However, a review of the results 14 years later suggest that quite the opposite has happened.
Among other benefits, Portugal has seen a reduction in “past year” and “past month” drug use; a reduction in a dramatic decline in HIV and AIDS in drug users, a reduction in crime; a reduction in addicts in prison and a reduction in drug deaths. This has clearly been an extremely successful policy.
So what happens in Portugal when you are caught with 10 or less days supply of an illicit drug? Your case is referred from the Ministry of Justice to the Ministry of Health (a huge shift in and of itself) and you appear before a drug dissuasion committee. You may be fined, but more often are not and you are offered treatment for your addiction, part of which included social re-integration. Their rate of drug addiction has fallen in half since the implementation of the policy.
Ah, but these programs are expensive aren’t they? Surely it would cost a lot to provide this service for addicts. You mean more than the $117,000 a year we currently pay to incarcerate them? Which, as is proven, doesn’t work.
As mentioned, I was a true believer in the war on drugs, but at the end of the day, as a physician, I have believe in an evidenced-based approach. The evidence shows that incarceration doesn’t work, and decriminalization with offers of treatment do. It’s time to ignore dogma and act in the best interests of Canadians. It’s time to end this war.













