Lots of talk on the net about how the economic model for family physicians no longer works in 2024. My own blog site has had guest posts dedicated to this issue. There has been some criticism of this position. Dr. Darren Larsen in a reply to the post linked above suggests he is “not seeing or hearing…ideas for solutions“. He further states that all paying doctors more will do is create a “better-paid, unhappy professional. Nothing has changed.”
Others have made the similar comments. There is nothing philosophically wrong with the argument to reduce workload instead of raising pay. Practically speaking however, history has repeatedly taught us that the Ministry of Health (MOH) bureaucracy is incapable of delivering on that promise.
Some personal stories:
In the mid 2010s I was a Peer Lead for OntarioMD (no really!). I was frustrated by the Ontario Lab Information System (OLIS) because I had to manually retrieve all the lab work for a patient individually in their chart. Hospital Report Manager (HRM) by comparison, sends reports on all my patients directly to one inbox. (why we need two systems – and now more, is another story). The then VP of OntarioMD informed me they were working on “Practitioner Query” – which would allow me to get all my lab work from OLIS in one inbox. This was supposed to be ready in six months. That was over a decade ago.
From 2014-2018, thanks to the vision of my colleague Dr. James Lane, we developed an integrated health portal as part of our Health Links project for South Georgian Bay. For $35K a year, we were able to ensure that nursing homes could message physicians on their EMR. We dramatically reduced paperwork for physicians from nursing homes, improved health care outcomes, and reduced hospitalizations thus saving the entire health system money.
The MOH bureaucracy couldn’t wrap its head around this and wouldn’t allow it to continue.
For those of you who think I should have told people about this project, I wrote an article in the Toronto Sun about it. Afterwards, I got invited to do a presentation on this with the then CEO of eHealth Ontario and her senior team. Heck, when I was a keynote speaker at OntarioMDs Every Step conference in 2019 (no really!) I presented this project. The then head of the MOH Digital Health Team was there and heard it. Still, the bureaucracy couldn’t see their way towards allowing a project that saved physician time (and improved health care outcomes) could continue.
Ok, ok, so this blog is just for me to complain about not being listened to right? Well no, there are multiple other examples.
One workload issue for family physicians is keeping track of which of our patients get immunized for which vaccines. If only there was a central tracking system that sent the information to us directly. Wait, there is! The Covax system for tracking Covid vaccinations. Obviously the easiest and most sensible thing to do is expand the already existing system to add all the other vaccines so we get notified (eg when public health gives Gardasil). Yet 3 years after Covax, the MOH can’t even make this simple common sense change.
More? When I was on the SGFP Executive, one of our senior physicians told us the story of how he was on a working group to make the schedule of benefits (the fee schedule for Ontarios doctors) easier. After six months of meetings, they made a decision to add a comma to the descriptive sentence of one code. One comma in an 800 page schedule.
I could go on but you get the point. It’s fine for the MOH to say that that they promise to reduce the Admin burden for family docs. But frankly to these aged and cynical ears, it just sounds like them saying “This time we really mean it, honest!” – kinda like when Lucy promised to hold the football down for Charlie Brown for real this time, with predictable results.
Look, we have a five alarm crisis in family medicine in Ontario. Just about every week brings a story of another physician who is struggling with the economics of running a practice, and is considering quitting.
As with all emergencies, we need to have an effective triage system in place. Deal with the most urgent thing first, then go on to other things. We clearly can’t wait until 2034 for the MOH to implement some of the workload reducing schemes they might have (and no matter how much they promise they really mean it – it will take that long). So the first thing that needs to be done is bring financial stability to family practices so that they can continue to function while we sort out everything else.
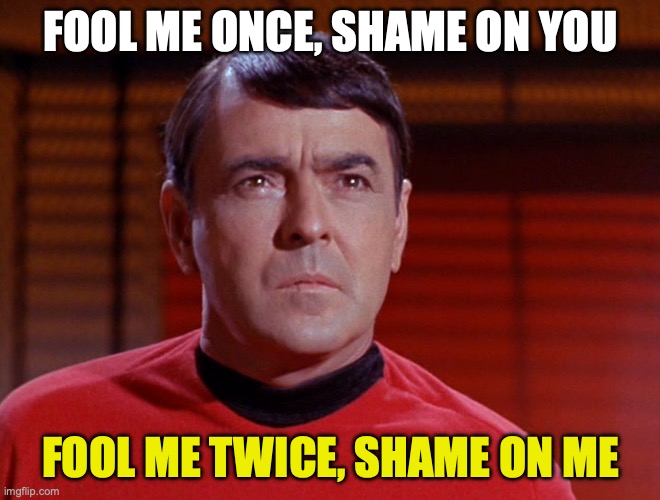
Now, given Ontario physicians are in the midst of negotiating a new contract with the Ontario government, I expect the MOH team to say to our own negotiations team something like – “I know you guys want X% increase, but we can only give you 1/2 of that, but we promise to reduce your admin burden so you are working less hard”. I would do the same if I was them.
But, my expectation, and the expectation I think of the majority of doctors in Ontario, would be that the OMA negotiations team looks at the MOH team, and quotes the best engineer in the history of Starfleet to them.
The first step towards fixing the crisis in family medicine is a new physicians service agreement that stabilizes family practices. Once that’s done, work can begin anew on health systems transformation/workload reduction and so on. To try to do it the other way round, or even hand in hand, is a recipe for further collapse of the health care system.


Oh Dr Gandhi, you touched the spot with this one. Any CEO from private business would fire whole ehealth or OntarioMD on a spot. Just take a look at ehealth sunshine list. What did they achieve in the last 3 years??? Trying to do an e-consult and it is a bad trip of multiple logins via outdate oracle software. Same people on different board wasting taxpayers money. MOH need to send them to UK to learn from EMIS, Accurex and docman how modern ehealth should work.
LikeLike
I don’t think money will change things much. I think we are underpaid and this has gotten worse with the various cuts and freezes over the last ten years. But we still do pretty well compared to many other professions. All the literature on happiness at work and income suggests that above about $100 000, changes in income don’t make people a whole lot happier. Sure, there is the expectation factor and the feeling of being paid what you are worth, which likely puts that number a bit higher for docs but the difficult factor to wrap one’s head around is that money doesn’t matter that much.
You can argue that money shapes the system and the system design has a greater impact on job satisfaction and I will accept that argument to a degree. But I don’t think we see huge differences in satisfaction between the current quite widely ranging funding models in Ontario (from FFS at the one extreme to salaried work at a CHC at the other).
But if money isn’t the answer then what is. Reducing admin work. Likely not. You have made some good points about annoying and time consuming admin work but the work you have mentioned happens almost subconsciously for most of us. We aren’t away of the stupidity that shapes our EMRs. We know they don’t work but we just roll that into our day. My HRM is a disaster due to my ER work. I get hundreds of messages a week on labs and imaging that I reviewed in the moment in the ER. Worse than that, I get duplicate copies of all of it for some reason. The IT guys have no idea why and can’t be bothered to fix it because it only affects a few of us who do large volume ER work but also have a family practice so also have an EMR. This kind of system admin hassle is not going to change (as you have outlined quite well) but I don’t think it is what most family docs mean when talking about admin work. I think they mean stuff like back to work letters, pre employment physicals, innumerable insurance forms, specialists with their own special referral forms, etc. The problem is that the government really can’t do much about these make work projects. They had legislation during the pandemic to limit work notes which was good but lost the plot after and bowed to industry to make us truancy monitors again. This burden can’t be changed without massive changes in broad categories of regulation. So it ain’t gonna happen.
So how do we get family medicine back in track? Back to basics. The relationship between the doc and the patient. We need to define what that does and doesn’t mean. Everything that isn’t in that core relationship is gone. Stupid metrics that don’t matter to Joe Smith, gone. Restrictions of evidence based meds by LU codes, gone. Committees to reform everything except the core relationship, gone. Eventually stupid insurance firms would also be gone but that would take longer.
I think we are way off the mark in all our discussions of what would make us happy again. What excites you about work? I bet it’s the patients. We need to focus on that! Until then, it’s all noise.
LikeLike
Sohail – I both agree and disagree with you on this.
When it comes to reducing administrative burden, the four tactics are
1) Eliminate
2) Minimize
3) Standardize
4) Automate
General principles that inform how we execute those tactics
1) A family physician should NEVER have to collect data from a patient beyond what is required to meet the standard of care.
2) Family doctors are NOT Commissioners of Oaths whose job it is to authenticate a person’s claim that they had an illness that prevented them from working/attending school etc.
3) Information requests from patients or third parties MUST be limited to copies of encounter notes and reports – they must seek opinions by referring patients to a team that they assemble, organize and pay.
4) There should be only one province-wide form for each situation, just like we have (almost exclusively) a single lab form. One imaging form, one form for non-lab/non-imaging tests, one form for each medical/surgical specialty, one initiation of disability form (follow-ups will be through an infrastructure paid for and maintained by the patients/third parties).
5) All EMR systems must be engineered to autopopulate the standard forms, limiting physician effort to a quick review and an authorizing signature.
I definitely agree that principle 5 will take time that we can’t afford.
But while items 3 and 4 require some system reform, the standardizing of forms and requiring the absence/disability system changes can be done in 6-12 months if the government forces the parties’ hands.
However, principles 1 and 2 are simply regulatory changes that they government can introduce in a heartbeat.
The bottom line: Family physicians need to stop letting the perpetrators of work burden off the hook. Ignore impassioned claims from whomever claims this can’t be done and tell them to just do it. Now.
LikeLike
Hey – certainly agree with your suggestions that there is stuff that can be done in the here and now. My frustration is that I tried to convince the powers that be when I was with OMA – and – well nothing happened. Which is why everything you say is important – my personal feeling is stabilize family practices financially first then……
LikeLike