NB. I am a consultant for Medicte, a medical tourism firm that connects people with the Acibadem Health Group in Turkiye. I appreciate my two loyal fans may read this to be an “advertorial” – but it does represent how I feel.

Recently, Leger released the findings of a survey that polled Canadians on their thoughts about the health care system. 70% of Canadians worried about not being able to get high quality health care. Surprisingly, only 37% thought the health care system was poor – did 63% not need medical care recently? But the number that should demoralize all of us is that only 17% feel the system will improve.
Like everyone else of a certain age, I’m coming to the realization that the one fight I won’t win, is the battle against time. More of my friends and colleagues are developing health issues. While I’m blessed to be in good health, like 83% of Canadians, I realize that the current health care system (which doctors call horrific and inhumane ), will not provide the access and care we should expect as standard in this country. I can only see things getting worse in the near future.
It does not help that I live in the health system every day. I’ve watched patients I really care about suffer in ways that I would not have imagined possible. Young people with cancer not getting treatment for three months. People with joint pain waiting a year for surgery. Patients developing complication after complication while on wait lists to access necessary treatments.
Most heartbreakingly, I see the toll that the burnout of working in such a hellishly damnable health care system is taking on doctors, nurses and other allied health care professionals on a daily basis.
That’s why I recently made the decision that if I, or someone in my family needed health care, I would seek care outside of Canada. I am not alone in this. The data is hard to get at, but going back as far as 2014, between 52,000 to 217,000 Canadians were seeking health care outside of Canada annually.
There are a variety of reasons to seek care outside of Canada, and specifically Türkiye:
- Getting immediate care. I could get hip surgery next week, not next year. Cancer patients get all the tests they need done within a week, not three months like I’ve seen.
- Getting treatments that are not available in Canada. Canada offers a host of great medical treatments, but many are not covered by government plans. Lap Band surgery is one. New, emerging radiation therapies for pancreatic cancer is another. There are more. All of these are available in Türkiye.
- Getting better allied health care support. Canada has GREAT nurses and other allied health care workers. But the system does not let them care for patients the best. Last time I was on call at my hospital, I overheard the nurses talking about how they each had 7 patients to look after for the shift. The safe number for an acute care hospital ward is 5 patients per nurse. We have excellent nurses but if you are constantly working at 40% over capacity, things are not going to go well. At the Acibadem hospitals in Türkiye, they have 4 nurses for 15 patients (3.75 patients per nurse).
- More cost effective care. I’m fortunate I can afford to pay out of pocket for care if needed. Worst comes to worst I’ll put off retirement for a couple of years to pay for things if necessary. But even I would have trouble with $200,000 (U.S.!) that B. C. resident Allison Ducluzeau spent on her cancer care. Costs in Türkiye for most procedures I looked at are generally less than half of what it costs in the U.S.
- First World Standards for Health Care Treatments. All of the Acibadem hospitals are JCI Accredited (the global leader in health care accreditation agencies). This puts them on par (and in some cases better) than top European hospitals.
- Türkiye is a well sought after Medical Tourism destination. Medical Travel Market recently highlighted 12 reasons why Türkiye was so well sought after including cost, world class facilities and cutting edge treatments. 1.2 million people went to Türkiye for medical tourism in 2022, mostly from Europe.
As part of my consulting work, I went on a fact finding tour to Türkiye and visited the Acibadem hospitals. To say my jaw dropped would be an understatement.

The hospitals (there are 21 in the Acibadem group) look like hotels. Each room is private. The wards are immaculate. All of the staff were incredibly attentive (and yes, spoke English).




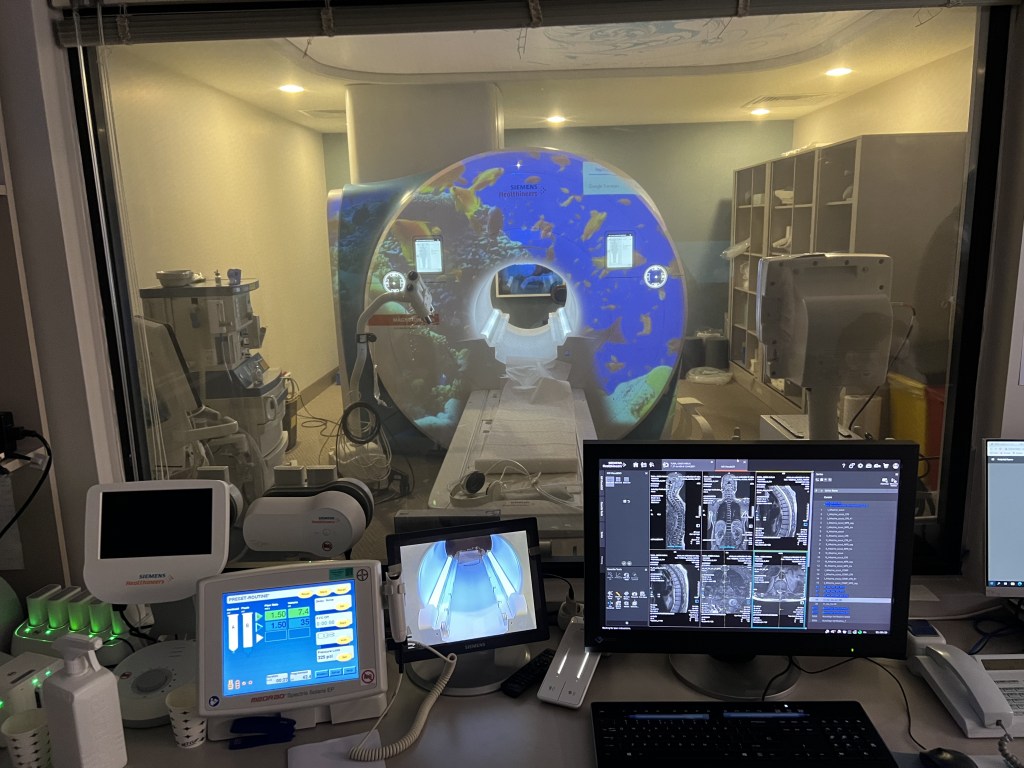
I asked to see the MRI, and the staff wanted to know which one (!). Their approximately 170 bed hospital had THREE MRIs, specialized for different conditions. This is on top of the CT scans, gamma knives (cancer treatment), PET scans etc etc. All of the equipment was brand new. I especially liked the MRI that projected a movie onto the equipment, to help children stay calm during the procedure.



I also ran into a couple of top ranked Turkish footballers (soccer players) while there. The Turks are as crazy about football as we are about hockey. Their top athletes go to the Acibadem group.
But what’s more impressive than the top ranked doctors, nurses and equipment is their philosophy of how to provide health care. If you were to sadly, get cancer, you would see all the specialists you need to see (surgeon, medical oncologist, radiation oncologists etc) on the same day. Any tests you need would be organized sequentially and rapidly over the next couple of days (if not the same day). You would have a full treatment plan within a few days.
Contrast this with Canada where you have to have an appointment with one doctor, then wait x number of weeks to see another then x to see another like my patients currently do. All while the cancer continues to grow.
Also, for the record, I did wind up getting care myself at Acibadem. Bad teeth run in my family, and so I went for a dental check up. The dentist examined me, put in two fillings, got the oral surgeon to come by and took out two teeth that were beyond hope, all during the same visit. This would have taken multiple visits in Canada. You could say I put my money where my mouth is. And yes, the care was excellent.
I appreciate this sounds like an advertorial. But the reality is that more and more Canadians are getting frustrated with the long waits for health care and seeking care outside of Canada. It may have started off with people seeking lower cost cosmetic surgery, but now things like orthopaedic surgery, cancer treatments, organ transplants, dental implants and even cutting edge infertility treatments can be had for those willing to travel.
There is never a guarantee of a successful result with medical treatments anywhere (including Canada). If considering leaving the country for care, people should do their due diligence. Make sure you deal with a reputable firm and first rate hospital.
I’ve made my decision, and I know where I’ll go.
If you or anyone else would like to explore options for out of country health care, contact Medicte for a free consultation.