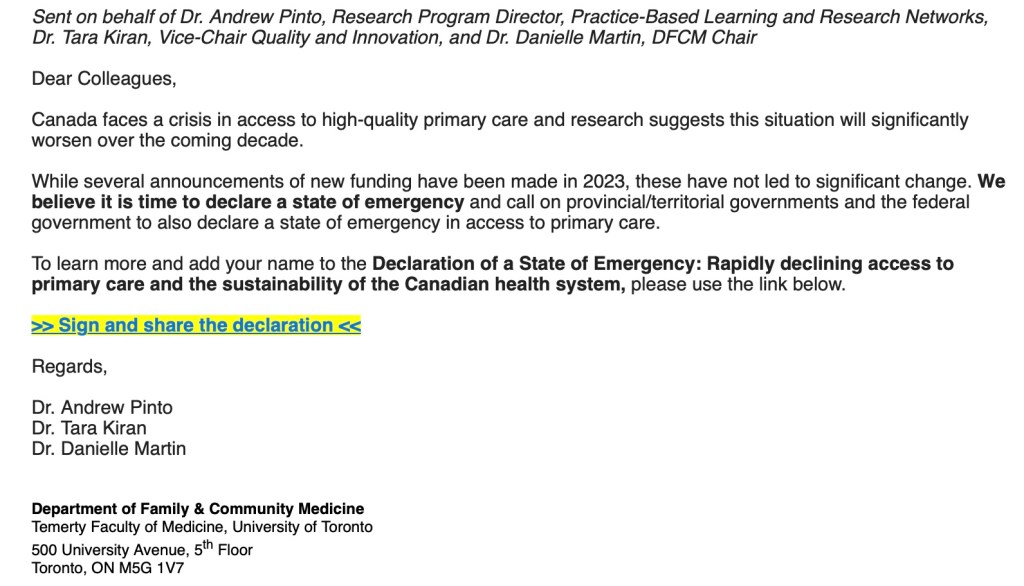
The following letter was jointly written by the three of us and published in the Toronto Star on February 20, 2024. It is being reproduced below so that we can share the letter on Facebook as we believe it will be of interest to physicians across Canada.
To All Family Medicine Residents,
We are writing to say congratulations! You are nearly at the end of a decade of hard work, perseverance and sacrifice; ready to start your career and “real life”. You have joined a beautiful and unique specialty. You will be the key to the healthcare system. You will find answers when patients arrive with ambiguous symptoms. Others will tag in and out of a patient’s health journey. You will stay and be an essential part of the beginning, middle and end of every patient’s story. You will save lives.
Your skill and knowledge are unparalleled, and there is no substitute for your expertise.
Which is why with heavy hearts, we, the undersigned, recommend that you do not start your own family medicine practice in Ontario. Not right now.
Family medicine is in crisis. Family doctors in Ontario are unable to provide the care they could and should. We face unprecedented levels of administrative burden, unsustainable business expenses, lack of healthcare resources, lack of social and cultural support for our patients and ourselves and finally, a lack of respect. This has led to widespread burnout and exhaustion.
In short, it is becoming frankly unsafe to run a family practice in Ontario, especially for those just starting.
We are family doctors with decades of experience. We are also physician leaders, past-presidents and board directors of the Ontario Medical Association (OMA), academic faculty, and health policy experts. We understand the situation well.
Do not sign that contract. Do not sign a lease, hire staff, buy equipment, contract with an EMR or any of the million things that must be done so that you can start a comprehensive care family practice.
Starting a practice at this time will require you to continue to sacrifice everything else in your life. If you have debt, you may not be able to pay it down, let alone start living the life you and many others have postponed for so long. You will struggle to spend time with your family, buy a home, care for vulnerable loved ones and more. You will continue to work at a non-stop pace, this time with no end in sight.
You will burn out and like many others, leave family medicine for good. This is why millions of Ontarians no longer have a family doctor.
The Ontario Ministry of Health can solve this crisis.
Governments in Manitoba, Saskatchewan and British Columbia have done so. This past year, they made family medicine a priority – and backed their words with targeted funding toward key programs to support both new and established doctors. It comes as no surprise that they have welcomed hundreds of new family doctors into their communities.
If they can do it, so can Ontario.
What can you do in the meantime? Work in hospitals, hospices, operating rooms and long-term care. Work in obstetrics, anesthesia, as a hospitalist, in emergency or palliative care, oncology, sports medicine etc. Be a locum. Bide your time.
You are skilled, smart, and adaptable. Your knowledge is extensive, demonstrating an unmatched depth and breadth of training. Use it.
When people leave comprehensive care family medicine, they almost never come back.
We don’t want that to happen to you. When the government of Ontario recognizes family doctors as the foundation of medical care, negotiates a fair contract and improves health policies to reflect patient needs in 2024… well, when that happens, we will write a different letter and welcome you to the world you were meant to be in.
We hope by then it is not too late.
Sincerely,
Dr. Nadia Alam, comprehensive care family physician and anesthetist, past-president of the OMA
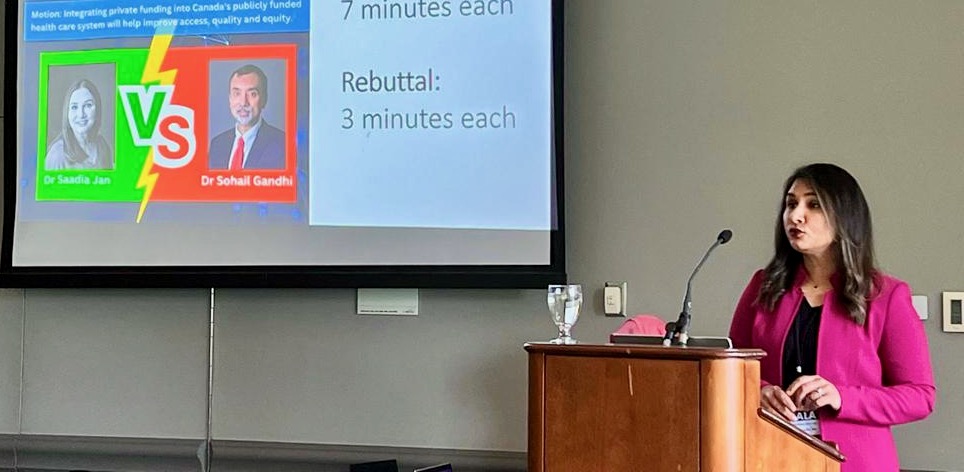
Dr. Sohail Gandhi, comprehensive care family physician and hospitalist, past-president of the OMA
Dr. Silvy Mathew, comprehensive care family physician and long-term care, past-board director of the OMA