Canadians want a high functioning health care system. This requires (but is not limited to):
- appropriate funding
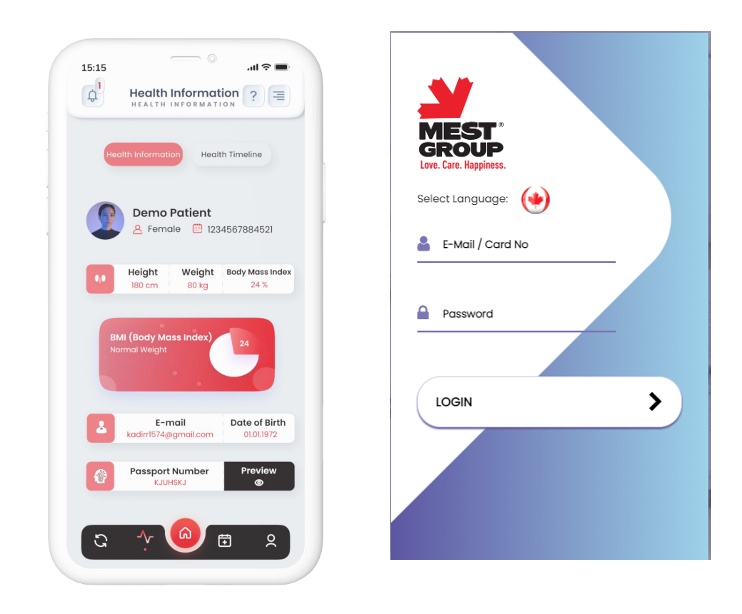
- a seamless electronic medical record
- strong support for Family Doctors (the back bone of a high functioning health care system)
- a “Goldilocks” level of oversight to ensure the needs of Canada’s diverse areas are met
- and much more
But one essential feature that is not talked about nearly enough is patient accountability.
Doctors diagnose and treat patients. More of us (thankfully) are also discussing proactive measures to prevent people from getting sick (appropriate screening, lifestyle tips, advice on menopause/andropause etc).
BUT patients also bear a vital responsibility in their own health outcomes. When patients are accountable—meaning they are informed, engaged, proactive AND use the health system appropriately—health systems perform better. In contrast, passive, non-adherent patients who misuse health care will strain health systems.
What exactly is patient accountability? Partly it’s the degree to which individuals take responsibility for managing their health. This encompasses adherence to prescribed treatments, lifestyle choices, attending medical appointments, following preventive care recommendations and so on. Certainly patients who adhere to current guidelines for, say, diabetic care, will have fewer complications and wind up in hospital less and use health care resources less overall. This is why investing in proactive teaching for diabetics has been shown to not just improve health care outcomes, but also the cost to the health care system.
Patient accountability cannot exist without adequate health literacy. Patients must understand medical terminology, navigate health systems, and assess risks to make informed decisions. Without health literacy, patients cannot be expected to manage their care effectively. A diabetic patient who learns to read food labels, monitor blood sugar, and adjust insulin levels exemplifies accountability in practice. When one looks at just how disjointed our current health care system is, it is clear we have much work to do to improve health literacy amongst our patients – and that dollars spent to promote this, will be money well spent.
But patient accountability also refers to how patients use the health care system. Our health system is under pressure from growing demand, finite resources, and rising costs. Patient accountability plays a pivotal role in mitigating these challenges.
Non-adherence to treatment alone is estimated to cost billions annually in avoidable hospitalizations, emergency room visits, and disease complications. For example, failure to take antibiotics properly can lead to resistant infections requiring more intensive care. Likewise, patients who frequently miss appointments or use emergency departments for non-urgent needs place undue strain on systems designed for more acute care.
By contrast, when patients manage minor issues at home, access preventive care on schedule, and comply with physician recommendations, they reduce unnecessary utilization of high-cost services. This not only frees up resources for patients with more serious needs but also ensures that funding is directed toward value-based care rather than avoidable interventions.
During my time in practice, I have only seen one government paper that talked about patient accountability – the (in)famous Price-Baker report of 2015. Written by lead authours Dr David Price and Elizabeth Baker, and including luminaries like Dr. Danielle Martin on their expert committee, one of it’s ten principles stated:
“The system is built on joint accountability: Each primary care provider group is responsible for a given population and their primary health care needs. Both provider groups and citizens are expected to use the system responsibly.”
Since then of course I have yet to hear Drs. Price/Martin or any of the other authours talk publicly about patient accountability.


How does this work in other countries?
In Finland, patients are told they have the right to good care that respects their opinions and ensures that there is informed consent with treatment. This onus is on the doctors. BUT, Finland also puts accountability measures on the patients in the form of user fees. They are generally nominal, but they are there, and I would suggest, serve to make patients think about whether they are using the health system wisely.
In Norway a similar concept applies. Health care is heavily subsidized by public health insurance. However there are user fees up to a prescribed annual maximum (currently around $250 if I’ve done the currency conversion correctly). After that, all your health care needs are covered (nobody goes bankrupt if they get cancer).
Then we have the Netherlands. There you are required by law to purchase health insurance (there are many providers apparently). There are various packages from basic to more comprehensive and the costs vary. There is also, unsurprisingly, a deductible, known as Eigen Risico, which you have to pay, before your insurance kicks in. It’s mandatory.
I picked these three countries as examples because not only do have a reputation for providing excellent health care, but because they are often talked about in glowing terms by the two physicians who seem to be driving the change in Primary Care in Ontario, Dr. Jane Philpott (Chair of Ontario’s Primary Care Action Team) and Dr. Tara Kiran (principal investigator for the ourcare.ca project)


Dr. Philpott frequently mentions countries like Finland/Norway, not just in her book (Health for All) but in various interviews. Dr. Kiran has frequently mentioned the Netherlands. They have generally spoken in glowing terms about how well the health system works in those countries and how almost everyone has a family doctor there.
I’ve also never heard them talk about how those countries require patients to be accountable for how they use the health care system.
Currently, our health care system is poorly rated compared to its peers. Canadians want, and deserve a better system. But in order to get that, we need to recognize that preserving our health care system is a shared responsibility. Despite what the politicians say, you should NOT be able just to walk into a health care facility and automatically expect it to be perfect. Rather, we should all recognize that we taxpayers own the system. As owners, we have a responsibility to use it fairly, wisely and appropriately. And yes, that means putting in mechanisms like deductibles to ensure people think about how they use health care.
Or we can carry on with a health system in a perpetual state of crisis. The choice really is up to us.