Gonna try something a little different. Over the years I’ve often found that there are a number of small stories that happen in a a week that are not worthy of a blog, but worth disseminating. So every Sunday (fingers crossed) I’ll try to collate (briefly) some stuff that happened in the past week in health care, along with my thoughts.
Item: Government of Manitoba announces a large number of health care workers (including 116 NET new physicians – a new record) have moved to the province in the past year.
My thoughts: It just goes to show you how a province and its residents benefit when government’s treat physicians fairly and come to a deal rather that dragging things out through an acrimonious arbitration processes. The second thought is it goes to show the political spin around health care will never end. It was the previous Conservative government of Heather Stefanason that signed the agreement with Doctors Manitoba that has bolstered their physicians population. New Democrat Premier Wab Kinew taking credit for this is somewhat laughable, but let’s face it, if the situation was reversed, the party in power would do the exact same thing.

Item: Private physician social media sites are complaining about some sort of change at the Pharmacy and Administrative level at Ontario Health around processing orders for palliative patients. It’s taking much longer for symptom relief kits, pain pumps, subcutaneous medications and the like to arrive. Hasn’t affected me or my patients yet, but apparently new process means that you have to have all your orders in place by 1:00 pm for them to get done on the same day, and stories are popping up in physicians facebook groups about patients suffering and nurses not having the tools to do their jobs.
My thoughts: It’s not a problem. I’ll just tell all my palliative patients that they are not allowed to de-compensate after 1:00 pm on weekdays and never on weekends. That’ll fix it.
Item: Yet another excellent op/ed written about how difficult it is to get a family doctor in Ontario and how you shouldn’t need a “golden ticket” to get one.
My thoughts: Honestly don’t know what it’s going to take for the government to take some action on this issue at this point. Or for the public to march on Queen’s Park daily.
Item: Vice-Chair of the Ontario Pharmacists Association terminates her agreement with PrescribeIT over a funding dispute. I gather there is some sort of transaction fee now for pharmacists.
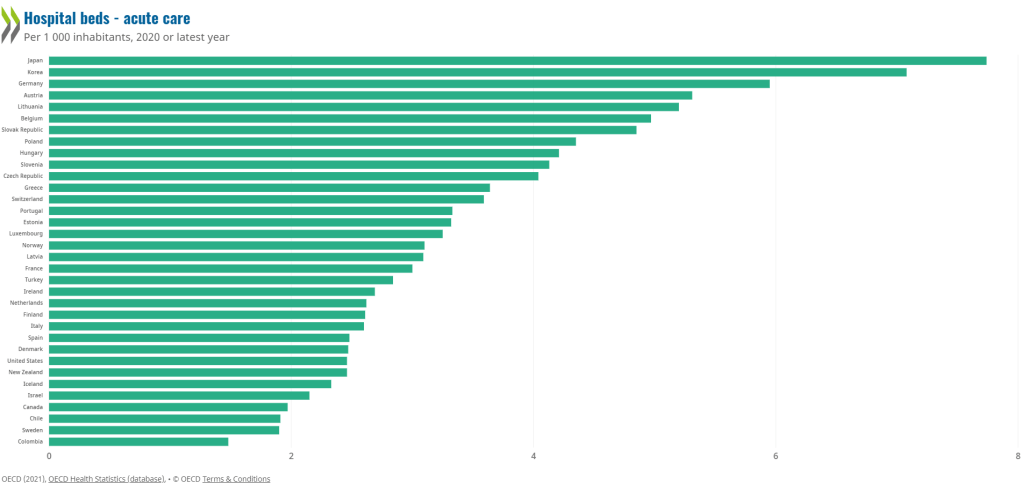
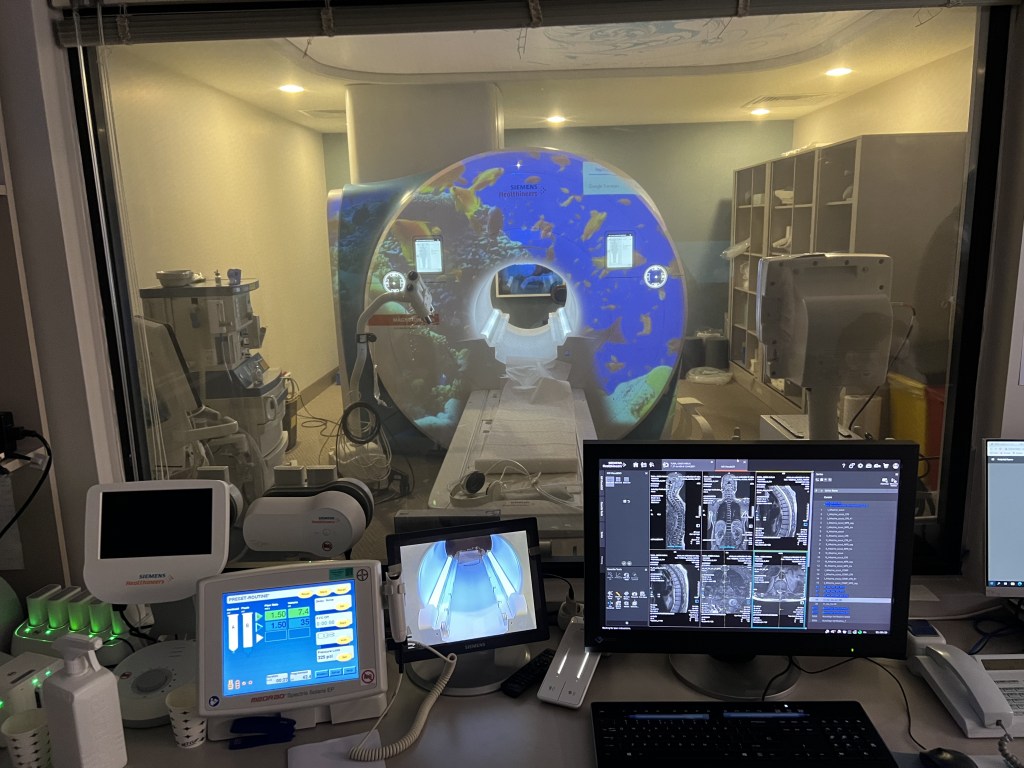
My thoughts: There are, huge benefits to having a completely integrated digital health system. I’ve referenced countries like Turkiye and Estonia before about this. Reality is thatmost advanced countries have integrated electronic health care (except the United States). The government should fund this – the savings will far outweigh the costs, if done properly.
Item: Dr. David Price responds to the criticism of him being chosen as a keynote speaker by the College of Family Physicians of Canada for their Family Medicine Forum.
My thoughts: I found it odd that his response included internal Ministry NTF processes. My understanding is that stuff was supposed to be ultra secret. In particular he mentioned a proposal was coming well before presented and announced. He didn’t specifically mention numbers per se. But he also seemed to back off supporting the 3% increase (which he isn’t allowed to do under team rules) or at least suggest it wasn’t his idea. If he was on the OMAs NTF he probably would have been kicked off for saying this stuff, but I guess the government, as always, plays by different rules. And saying he would be happy to not give the Keynote was……..strange. Oh well, at least it gave the chance to do this (and yes you can re-post from here if you want):

I continue to encourage all family physicians to sign the petition asking the CFPC to remove Dr .Price as a keynote speaker by clicking on this link.
That’s it for this week’s Sunday Snippets. A blog on how the Ontario government continues to attack family physicians coming in the next day or two. See you (hopefully) for more snippets next Sunday.