NB: This is a copy of a column I originally wrote for Postmedia in October of 2015. It’s copied here so that I can access it easily in the future. And a sad reminder that as of 2023, things haven’t changed for the better. If anything, they are worse.

Ontario’s health-care bureaucracy has exploded over the past 12 years, mostly because the government has set up a series of arm’s-length agencies it can scapegoat.
I’ve experienced this bureaucratic mess first-hand.
From 2013 to early 2015, I was the lead physician for the South Georgian Bay Health Links. I took the position because I was told the goal was to co-ordinate care between various health-care agencies to better help patients with the most complex illnesses.
Then-health minister Deb Matthews said there were too many “silos” in the health-care system and anointed her then-associate deputy minister the “silo-buster.” The ADM told us to develop a local solution — because each area is different — and focus on our strengths to help these patients.
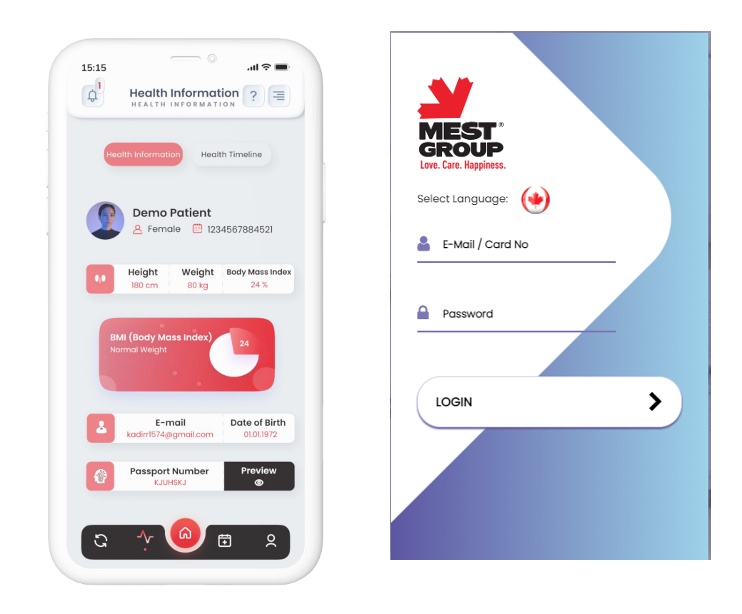
Our area is very fortunate to have an advanced IT infrastructure. Virtually all 60,000 residents have an electronic medical record (EMR) in a joint database. We are also one of only two regions in Ontario with electronic prescriptions. This process requires the pharmacy to have a portal that allows it to communicate securely, in real time, with the physician to discuss issues of clinical importance.
My patients have benefitted significantly from this technology, so our thought was to set it up with other allied health-care providers (home-care nurses, retirement and nursing homes, community support workers, etc).
The Ministry of Health funded Health Links through the Local Health Integration Network (LHIN). So we put a proposal together and took it to the LHIN. The LHIN’s IT department liked the idea, but wanted to get input from the ministry. The ministry liked the idea, but wanted us to get the input of eHealth Ontario, the independent agency trying to create electronic health records. eHealth told us to come to a “regional network meeting.”
At the meeting, they thought the idea was good, but asked for the ministry’s eHealth liaison to comment. The liaison referred it to the ministry’s IT group (yes, the ministry has both an eHealth liaison group and an IT group) who wanted to ensure compatibility with a “provincial solution” — even though we were told to develop a local one — and suggested we review with the LHIN IT department.
After a year of “circling back” (a phrase I learned from these guys that I came to detest) we finally gave up, funded the project ourselves for $70,000 — less than a salary on the province’s Sunshine List — and my complex patients are now starting to see the benefits.
As I have come to appreciate, the government set up these various arm’s-length agencies, such as the LHINs, eHealth, Health Quality Ontario, Community Care Access Centres and so on, rather than simply have the ministry accept responsibility for these tasks. From a politician’s point of view, this gives them the ability to deflect criticism by saying such and such agency is “independent.” For the most part, this has worked for the Liberals. They’ve won four elections in a row. But it certainly hasn’t helped the patients any.
My colleague, Dr. Shawn Whatley, posted a superb blog piece that looks at how many bureaucrats work in Canada’s health-care system. It shows Canada has three times as many bureaucrats as other countries with advanced universal-care systems. Even worse, Ontario has only 1.7 acute-care hospital beds per 1,000 people, which is about HALF the average for other OECD countries. Ontario got to this number by closing 17,000 acute-care beds — and laying off the nurses needed to staff them — between 1990 and 2013.
But at least the bureaucrats are producing meaningful reports and are happy to be helping with moving health system transformation forward, right? Not so, according to a recent survey of health leaders conducted by Quantum Transformation Technologies. Most respondents said they aren’t happy with Hoskins or the LHINs.
It’s dramatic just how badly health leaders feel the system is working. The comments at the bottom of the survey are equally telling. There are repeated calls to cut the number of LHINs and reduce the size of the bureaucracy.
So in summary, Ontario is burdened with a bloated, ineffective, and demoralized health-care bureaucracy.
Wynne and Hoskins’ solution to this? Lay off nurses and start a fight with doctors over their fees.
Franz Kafka couldn’t have come up with something this convoluted.
— Mohammad Gandhi, MD, CCFP, FCFP, is an assistant clinical professor at McMaster and Queens universities.
* More than 1,000 doctors recently joined a Facebook group to complain about how the Ontario Medical Association, which represents them, isn’t sticking up for them in their fee fight with the province.
Earlier this month, the province cut funding for doctor services by $235 million, chopping doctor fees by 1.3%.
******************************
GROWING HEALTH-CARE BUREAUCRACY
* There are 0.9 health-care bureaucrats per 1,000 people in Canada, compared to 0.4 per 1,000 in Sweden; 0.255 in Australia and 0.23 in Japan. Germany has 0.06 bureaucrats per 1,000 people.
* Ontario has only 1.7 acute-care hospital beds per 1,000 people, which is about half the average for other OECD countries.
*****************************
A recent Canadian Institute for Health Information (CIHI) report — the one Premier Kathleen Wynne and Health Minister Eric Hoskins say shows “Ontario has the best paid doctors in the country” — also says 12,000 Ontario nurses left the profession this past year.
* It also shows Ontario has only 176 physicians per 100,000 people (ranking 7th in Canada).
* Ontario has the fewest family doctors per 100,000 people out of all the provinces. Only 10% of family doctors in the province are accepting new patients.
* A recent Quantum Transformation Technologies survey of Ontario health leaders found 55% think Hoskins is doing a poor to fair job, 62% think the LHINs are doing a poor to fair job, and 50% feel the government has a poor track record of helping those with mental health issues.