Another in a weekly series of brief snippets of health care stories that bemused, intrigued and otherwise beguiled me over the past week along with my random thoughts on the matter.
Item: New reports show that marijuana use is linked to thinning of brains in adolescents.
My thoughts: It’s not just adolescents. And it’s not just brains. I’ve seen a marked rise in people with significant mood issues ever since marijuana was legalized. There has also been a significant rise in people with stomach/bowel issues in my practice that all other tests turn up negative for. Patients with these issues are invariably marijuana users and the blunt reality is they won’t get better until they stop. I continue to be in favour of decriminalizing marijuana and other illicit street drugs if and only if we do it the way Portugal did it and not the haphazard way it is being done in Canada. But we really need to re-think the full on legalization of it.

Item: A survey in Medscape showed that there were two factors critical to reducing family medicine burnout. First would be to reduce the Electronic Health Record burden, particularly the number of times family physicians have to chart from home. Second would be to build stronger physician/nurse teams. Crucially, the teams need to be led by the family physician and NOT a bureaucrat or some other team member.
My thoughts: I hope this finally gets the Canadian Medical Association (which despite over $2 billion dollars in their bank account is amazingly growing increasingly irrelevant to front line physicians) to SHUT UP ABOUT SICK NOTES ALREADY. That’s not going to solve burnout (even though I like every other doctor hate doing them). To paraphrase a political slogan – “It’s the Electronic Health Record, stupid.” My second thought is that I remain extremely concerned that while I do feel Dr. Jane Philpott is well intentioned in her new role (to lead a primary care action team) – the bureaucrats at Ontario Health will sabotage her. They will see “teams help”, then create teams that have the assistant to the secretary to the aide to deputy minister’s attache for the Primary Care Secretariat’s deputy vice president run them. That will be a disaster. Teams need to be led by family physicians. Full stop.

Item(s): The family physician crisis in Ontario continues to worsen. Tillsonburg lost four family physicians. Wallaceburg is launching a large physician recruitment program to deal with their shortage. Brantford is taking a more hands on role to get more family physicians. Brockville is hiring a consulting firm that employs former health Minister George Smitherman to help tackle their shortage.
My thoughts: It’s sad that we are in a seeming “Hunger Games” of one community fighting another for the precious resource that is a family doctor. If only someone had warned people a crisis was coming. Oh, right.

Item: Premier Ford promises to correct the mistakes at Ontario Health at Home that led to a large amount of suffering for patients. He also stated that the people who “messed this up” will be “held accountable”.
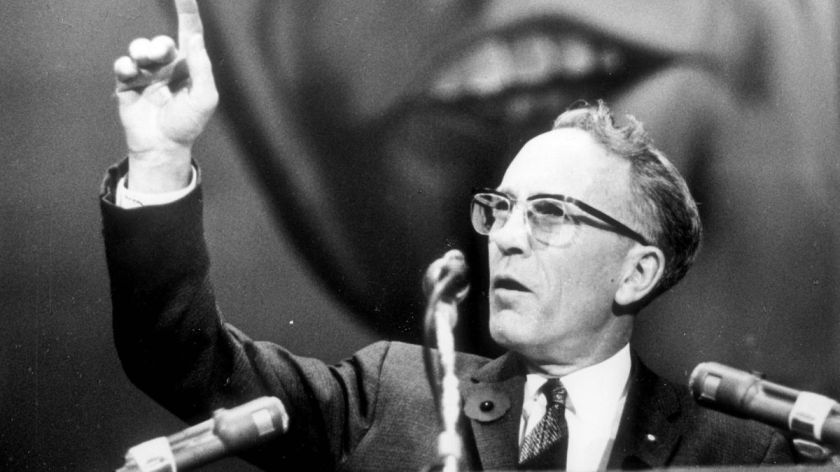
My thoughts: I’ll believe it when I see it. When I wrote about mismanaged bureaucracy in health care (back in 2015!) I pointed out that no decision seems to get made by bureaucrats without continuously “circling back” to one committee or another. The reason I’ve discovered, is because this way, no individual gets blamed for (the very many) bad decisions made in health care. I’ve yet to see a health care bureaucrat fired – and I’ve met many who deserved to be. I really hope that the comments by Premier Ford signal a return to the old Doug Ford who promised to end the “gravy train” and famously said:
“What drives me crazy is when you have a supervisor in government, and they report into 12 other supervisors. That’s unacceptable.“

Item: Male doctors are working less hours in a week than they used to. They are still working more than the average Canadian worker, but there has been an unmistakable decrease in how many hours they work
My thoughts: Finally! Proof that men are getting smarter! There’s more to life than work, and good for the younger docs – all of them – for seeking balance in their lives.
Item: A young Ontario mother died of cholangiocarcinoma (cancer of the gall bladder), after encountering multiple road blocks getting a new treatment (Pemigatnib) approved for her.
My thoughts: This story is absolutely infuriating and encapsulates what is wrong with our health care system. Look, there is no guarantee that she would have survived if she had gotten the treatment (it’s an awful cancer she had). BUT – look at all the regulatory agencies involved in getting the drug approved. Health Canada approved the drug in 2021. But the Canadian Agency for Drugs and Technology in Health said the evidence wasn’t clear. (So why then did Health Canada approve it?). Furthermore there are multiple provincial drug agencies involved, which means she could have gotten it had she been a resident of Quebec, but not Ontario (two tier medicine anyone?). It’s the bureaucracy and double speak from having too many agencies involved that angers me greatly. A wholesale streamlining of the process for medication approvals is desperately needed.
That’s all for this week. Back next week (probably) with more.