In 2004, the CBC surveyed Canadians to see who would take the title of “The Greatest Canadian.” The winner was former Saskatchewan Premier Tommy Douglas. Douglas is widely, and correctly viewed as the founder of socialized health care in Canada.
His selection speaks not only to the dramatic impact he has had on this country, but just how much Canadians value health care. I will dispense with calling it “free health care” because that just isn’t true. Our tax dollars pay for it. But those dollars are supposed to provide care for all those who need it.
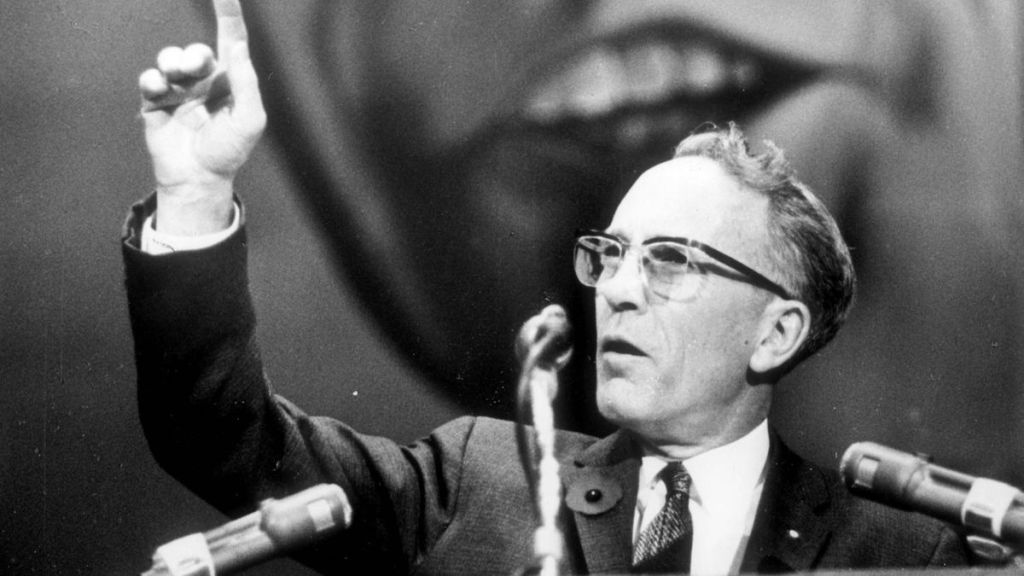
As our health care system continues to collapse all around us, it’s worthwhile, I think, to look back at the type of health care that Douglas envisioned. The truth of the matter is, that it is quite a bit different than what we have today. And I think, is not at all what Douglas would want.
According to “The Canadian Encyclopedia“, Douglas’ views on health care were shaped by a number of events in his early life.
As a six year old, Douglas fell and cut his knee. Unfortunately, he developed osteomyelitis ( a bone infection) and the consequences hampered him for his entire life. He had numerous operations and at one point doctors in Winnipeg considered amputating his leg. Fortunately, a well know orthopaedic surgeon (Dr. R. J. Smith) offered to operate for free, so long as Douglas allowed medical students to watch. This saved Douglas’ leg, and helped convince him that health care should be readily accessible to everyone.
Later, as a young man, he moved to Weyburn Saskatchewan, and was dismayed by the complete lack of medical care. He buried a 14 year old girl who died of a ruptured appendix because she couldn’t get medical care. He also vividly told of burying two young family men in their 30s, who simply couldn’t afford to get medical care.
These experiences helped to shape his belief that we could do better as a country. I would suggest that all Canadian should share the belief that one should not have to choose between going bankrupt (or dying) and getting basic medical care.
As premier of Saskatchewan, he implemented the Saskatchewan Hospital Services Plan covering the needs of patients admitted to hospital. In 1961, he implemented the Saskatchewan Medical Care Insurance Act, that provided medical insurance for all residents of Saskatchewan. This of course eventually led to other provinces and the Federal Government adopting similar programs.
The wording is important, and I think speaks to what Douglas was trying to achieve, and frankly, where I believe we need to go back to. The plan was “Insurance”. With all the benefits, AND RESPONSIBILITIES that go along with insurance.
Here’s the thing. In Canada, ever since the Canada Health Act, we have really deviated far from what Douglas really envisioned. He never ever wanted a system where you could go to any health care provider and get assessed without any responsibility on your part. Indeed, he spoke to that quite eloquently in the Saskatchewan Legislature on October 13, 1961:
“I want to say that I think there is a value in having every family and every individual make some individual contribution. I think it has psychological value. I think it keeps the public aware of the cost and gives the people a sense of personal responsibility. I would say to the members of this House that even if we could finance the plan without a per capita tax, I personally would strongly advise against it. I would like to see the per capita tax so low that it is merely a nominal tax, but I think there is a psychological value in people paying something for their cards. It is something which they have bought; it entitles them to certain services. We should have the constant realization that if those services are abused and costs get out of hand, then of course the cost of the medical care is bound to go up.”
Douglas intuitively grasped that if people perceive something as “free” they will start to lose their sense of using it responsibly. That’s why the initial Medical Insurance Act was just that. A form of insurance funded by the taxpayer, and like all forms of insurance, there was a deductible and reasonable limitations.
People were able to now access health care, for a small fee that allowed them to recognize that they too had to take some responsibility for how they used the system. They also had to realize that not everything was covered. Basic health care yes. Options like wanting, say, a private room instead of a ward bed in hospital – well that would be an extra.
There are many problems with the Canada Health Act. But the most fundamental is that it is based on the premise that you can endlessly get something (in this case health care) for nothing. Gutless politicians (from all parties) continue to promote this mantra in never ending attempts to woo votes as opposed to, you know, actually telling the people the truth. Namely, that people should take some responsibility for how they use the health care system.
By continuing to perpetuate the the lack of accountability, our cowardly politicians have created a culture of entitlement instead of a culture of empowerment. Many (not all) people believe that they should be able to get all manner of testing because it’s “free”. I’ve been blessed to have a very pragmatic practice in general, but even I have had to tell people that I will not be ordering the serum rhubarb levels their naturopath wanted because it would be “free” if I ordered it instead of them, or the full body MRI that some “wellness consultant” asked for.
It’s time to bring some patient accountability back to health care. And the first step in that would be to go back to the model that Tommy Douglas had proposed all along.