Health care is consistently viewed by Canadians as their number one priority in any federal or provincial election. It is the largest portfolio of provincial government budgets and is responsible for a substantial proportion of the federal budget. Yet despite all this expenditure, it continues to fail the citizens of Canada.
As I’ve repeatedly said in the past, our health system needs a bold and innovate transformation if it’s to provide care to Canadians in the 21st century. In a previous blog, I had promised to come with some ideas on how to do that. I submit the first step should be to make health care a federal responsibility, and not a provincial one.

I know, I know, this will require an amendment to the Canadian Constitution, a dizzyingly complex process. But I have an idea for that as well, that I will get into later in the blog.
For now, let’s look at just some of the reasons why we should have a National Health Care system.
Canadians Already believe we have a National Health Care system
Regardless of how the division of authority is laid out, the reality is that Canadians feel that no matter where they go in this country, they will get health care paid for by their taxes. “You shouldn’t need a credit card to pay for your health care” is a mantra that is oft repeated by politicians. It’s part of the Canadian identity say other pundits. Logistics aside, politically speaking, this simply is in keeping with what Canadians already think.
The Canada Health Act puts provinces in a no-win situation.
Somewhat unbelievably, I find myself defending some politicians here (I’m just as shocked as both of my loyal readers are). The argument presented to me by political leaders with whom I have spoken in the past was that premier’s don’t want Ottawa telling them what to do, or how to spend dollars. Certainly, we saw some of that in the wrangling over the most recent health care accord where premiers pushed back on simple things like data collection.
But I feel that it’s the premiers who are in a bind here. The feds can go around saying, “hey, we are going to support the five principles of the Canada Health Act” and then……well do very little about ensuring that. The premiers are stuck because they can’t violate the act. However, they have to figure out how to manage the system with declining revenues. And of course, take the flack when the system is failing.
It’s time to make the level of government that boldly proclaims that Canadians don’t have “pay out of pocket” for health care responsible for implementing it.
The efficiency of the system will increase
I’m serious (honest). Once again, let’s look at the most recent health accord. The federal government agreed to increase spending on health but in return requested health data management. In order to do so the feds propose to have “tailored bilateral agreements” with the provinces and territories.
That’s right, instead of having one team come up with a national data standard, there now have to be 13 committees to hash out how to do it. Which means, you guessed it, 13 times the number of bureaucrats. In 13 times the number of meetings. If the feds ran health care, they could just have one committee to oversee the changes for the whole country.
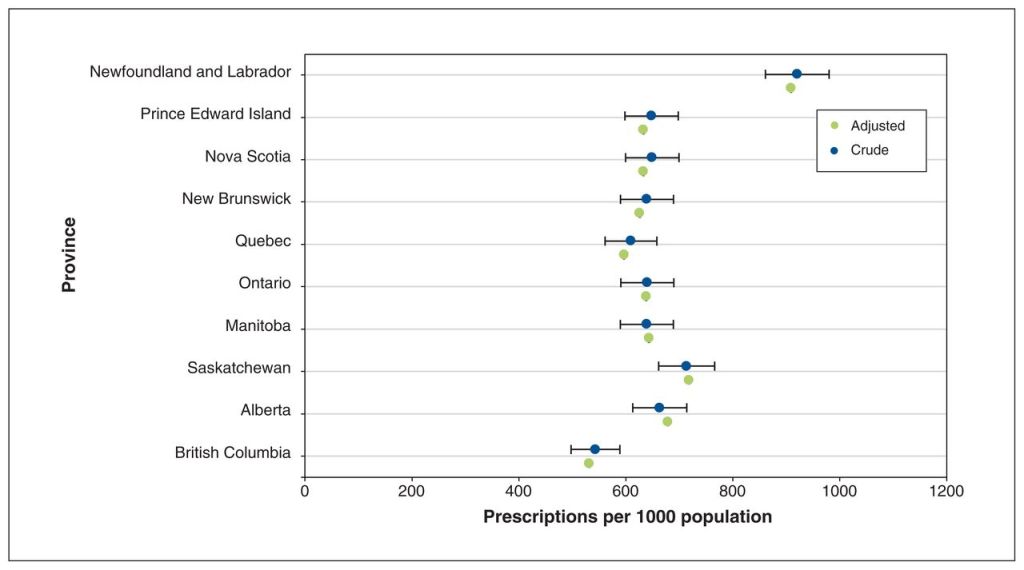
The same would apply to just about every other aspect of health care. Whether determining what services are covered (there is intra provincial variation), to determining things like public health policies and so on, a unified Canada wide health system would be far more efficient.
Who knows, they might even be able to take the money saved from having 1/13th the number of bureaucrats and invest that into hiring more health care workers………nah, they’ll probably put it into more $6000 a night hotel rooms for our effete Prime Minister.
Unified Rules/Licensure requirements across the Country
The Canadian Medical Association (CMA) is strongly advocating for pan-Canadian licensure to deal with the physician shortage (so much so they almost make it sound like a panacea). I support national licensure of course. Although I wish the CMA would focus on getting us pensions and getting the government to reverse the tax changes that so harmed physicians in 2017. That would really help their members (the ones they are supposed to be serving).
But let’s be real, national licensure ain’t gonna happen with 13 separate provincial regulatory bodies all trying to generate income to run their organizations with licensing dues.
BUT, make Health Care federal, and you only need one regulatory college that can set Canada wide standards (for all professions, not just physicians).
Similarly, programs like national pharmacare (the one then Prime Minister Paul Martin promised us by 2006) and other programs can all be implemented more easily.
So what are the next steps to take?
There are undoubtedly many other examples of what could run better with a single, Canada wide health system. The big question of course, is how do we change the constitution to allow this?
Canada is due for an election by 2025. It might happen sooner if NDP leader Jagmeet Singh tires of the foppish behaviour of our current Prime Minister and pulls his support for the “confidence and supply agreement”. I propose that whenever that election is, there be a referendum on altering the Constitution. (It would be better than having two separate votes).
Canadians would go to the polls, vote for the candidate of their choice, and then have a question to answer as to whether they support amending the constitution. Make it binding on the provincial governments. If there is Canada wide support for this, then the provinces would have no choice but to agree to the amendment (and as pointed out earlier, it would be better for them politically anyway).
Canadians have long viewed their ability to access health care without paying out of pocket as a quintessential Canadian quality. Having the provinces run health care may have made sense in the days of paper and telegraphs, when integration was nigh on impossible anyway. But in the 21st century, when integration is paramount to running a health care system, it makes no sense.
It’s time for the federal government to take over health care, so that the system can be run in the best interests of all Canadians.