Dr. Madura Sundareswaran once again guest blogs for me. She’s a community family physician who’s resume is too long to print here. She helped found the Peterborough Newcomer Health Clinic and is a recipient of the CPSO Board Award which recognizes outstanding Ontario Physicians. I happen to think she is one of our brightest young leaders.
I was feeling incredibly optimistic after Friday’s SGFP report, which articulated the importance of family physicians in addressing the current primary care crisis. But that hope was abruptly crushed by a recent email I received from Ontario Health East. Ironically, it serves as a prime example of how health systems transformation continues to follow a top-down approach with little regard for the realities of primary care delivery.
In its latest communication to its members, Ontario Health East outlines a two-step strategy for clearing the Health Care Connect waitlist.
Let’s talk about the good first.
Given that the Health Care Connect waitlist has been largely stagnant, the proposal to verify and update the list is reasonable and welcomed.
In its latest proposal, Ontario Health East also commits to providing “interim services” for patients who are not immediately matched to a family physician or primary care team. This is great – and arguably where the new “Care Connector” portfolio should focus. Why? Because this is what many Ontarians need right now: assistance navigating our complex healthcare system without a family doctor.
Now, the not-so-good.
A large part of Ontario Health’s plan is to connect with every primary care clinic in the OHT to determine available capacity. If I am reading this correctly, they want to cold call every primary care clinic in the region and ask if they are accepting new patients. Are they aware that people have been trying to do this for years…?
To their credit, Ontario Health has expressed a commitment to support capacity-building. They’ve emphasized exploring “creative ways” to expand capacity at the individual clinician level — but this language effectively masks the absurdity of the underlying ask. The expectation appears to be that family physicians, already working at or beyond full capacity, can somehow stretch further, simply by reimagining how we work — all while receiving little to no additional resources.
To their credit, Ontario Health has expressed a commitment to support capacity-building. They’ve emphasized exploring “creative ways” to expand capacity at the individual clinician level — but this language effectively masks the absurdity of the underlying ask. It assumes that family physicians already working at full capacity, can somehow stretch further, by simply reimagining how they work — with little to no additional resources.
I’d like to apply the trending analogy of comparing our healthcare system to the public education system.
Imagine 30,000 children in your community suddenly need a place in schools – all at once. Instead of building new schools, adding classrooms, increasing the budget for school supplies, or hiring new teachers – the plan is to call each teacher and ask if they can “accept a few more students.” Not just one or two students– try about 100 each. Now teachers, please brainstorm how you can better meet this need (on your free time, of course).
Parents and teachers – would you allow this to happen?
The dilution of services is not the solution to this primary care crisis. This government’s current focus is entirely on numbers – with little regard for the quality of care being compromised in this process. What happens when each of us have 100 more patients with little to no additional support?
- Less time for direct patient care as we dedicate more time to an overflowing inbox.
- Longer wait times to see your family physician.
- More strict enforcement of rules like “one problem per visit.”
- Even fewer family doctors choosing to practice family medicine. More choosing to leave or retire early.
Some argue that teams will offset this burden. Full disclosure: I do think teams can help. But whose responsibility will it be to create medical directives, identify how the teams can best work, and continue to engage in quality improvement and assurance as this new process evolves? Family physicians. Back to the classroom analogy – it doesn’t matter how many other support staff you hire, a classroom of 130 students needs more than one teacher.
This proposal assumes we haven’t already asked—more accurately, begged—family physicians to take on more patients. We have, many times. And with limited success. And before I’m criticized for being negative or dismissing innovation, allow me to share my own experience.
In 2023 I founded the Peterborough Newcomer Health Clinic with the intention of supporting newcomers to Peterborough transition to the Canadian Healthcare system. In this process, I follow newcomers for 6-12 months after which I personally cold call family doctors and primary care nurse practitioners to see if any of them will accept my patients after I have done a great deal of work completing intake assessments and consolidating all previous health records. I have already brainstormed and implemented strategies to make the transition as easy as possible. Have I successfully attached my patients? Rarely. Many of these patients remain unattached.
This is just one story. Many in our community — advocacy groups, primary care providers, and local organizations — have made similar efforts with limited success. And let’s not overlook the fact that this proposed model of attachment completely ignores the issue of inequitable access for marginalized populations (another post for another time).
As I sit here on a Sunday, preparing to enter the week without sounding like a “grumpy physician,” here are my final thoughts.
- In this race to reach 100% patient attachment to primary care; we must advocate to ensure that this is not done in a way that dilutes existing resources, compromises existing access to care and devalues family physicians who are currently working at full capacity. We need to protect our existing workforce and support sustainable growth. I encourage every user of our publicly funded healthcare system to advocate for this.
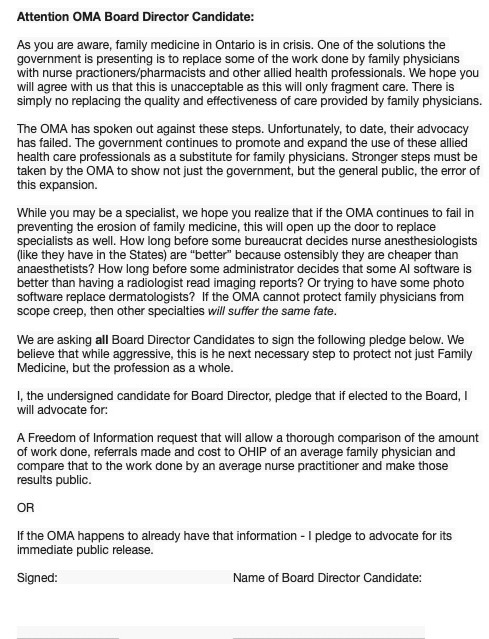
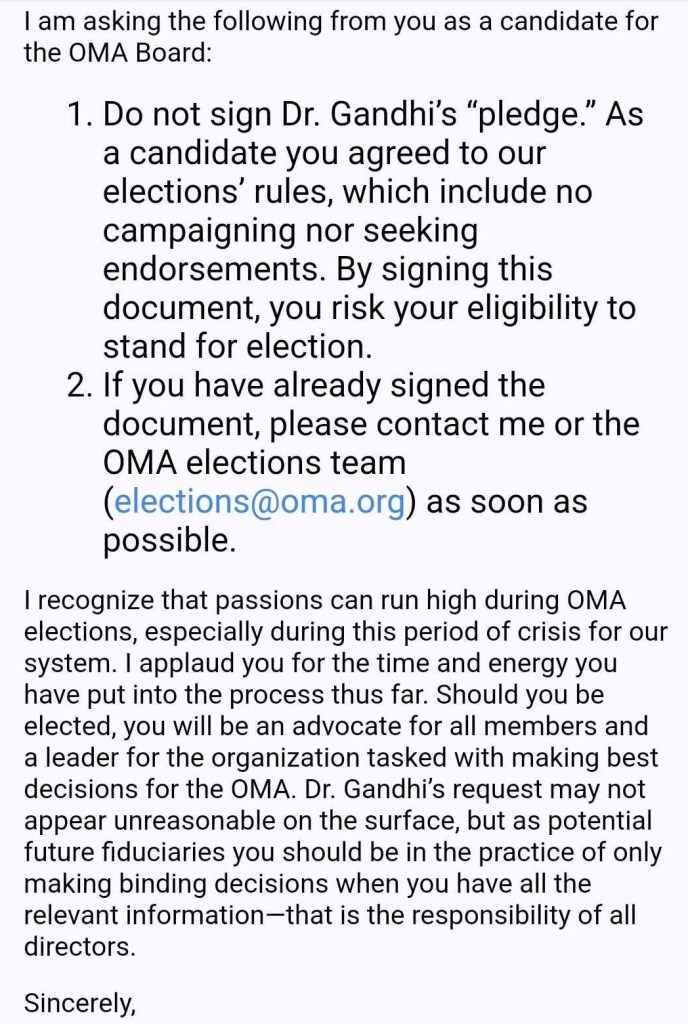
- Family physicians – I urge you to continue to advocate for better remuneration and exercise caution when pressed to roster more. Please remember that our contracts exist with the Ministry of Health and Long Term Care. When new opportunities arise – exercise due diligence to ensure that what is being asked of you aligns with the policies of your own practice/organization and the CPSO.
- Rushed, expensive, and poorly planned reforms that focus on quantity, not quality is not good for patient care. Failing to address the core issues with primary care – demonstrated by fewer and fewer family physicians choosing to practice comprehensive, community-based family medicine – is resulting in top-down, expensive, and band aid solutions to the primary care crisis. It edges on careless spending on taxpayer dollars. We should advocate for a system that prioritizes sustainable, safe and equitable care – not just a solution for tomorrow.
Disclaimer: The views expressed in this piece are my own and do not necessarily reflect those of any affiliated organizations or institutions.