Dr. Mark Dermer (pictured inset) , a recently retired family physician guest blogs for me today. He posted his thoughts about the arbitration process and how it can potentially affect family medicine on a private facebook group. I thought his post was excellent and I’m honoured that he has agreed to allow me to republish his thoughts here, so more people can see it.
A common misconception about how the arbitration decision will be determined is that the arbitrator will choose either the entire OMA submission or the entire MOH submission as the PSA award for 2025-28. While some arbitrations work like that – salary arbitration does – that’s not the case in the OMA-MOH 2017 Binding Arbitration Framework (BAF). As stated in paragraph 18 of that document (in this group’s files section):
“Absent an agreement of the parties, the method of binding interest arbitration to be used shall not be final offer selection. In particular, unless the parties agree otherwise, the arbitration board may, on any issue or issues, select either party’s proposal, choose a middle ground, or issue any award that it determines is appropriate in the circumstances.”
In other words, the arbitration board will issue a decision that is built point-by-point, with quantitative decisions set anywhere on the continuum between the two parties submitted positions. And the choice for each point/issue will be made in the context of the entire Physician Services Agreement (PSA).
For family physicians, there are four points of dispute that await the final PSA arbitration decision:
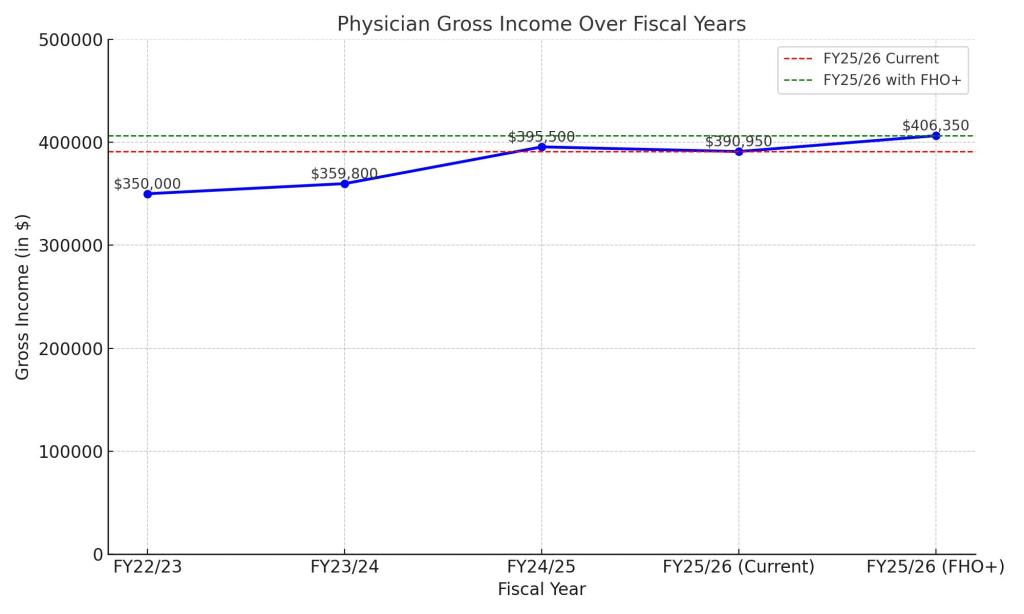
1) Annual increases to the Physician Services Budget (PSB) in years 2, 3 and 4 (2025-26, 2026-27 and 2027-28) of the present 2024-28 PSA. Note that these overall increases will then be subject to relativity adjustments that are managed within the OMA.
– OMA submission: 3.75% in each of the three years for a total of 11.25%
– MOH submission: 2.25% year 2, 2% in years 3 and 4 for a total of 6.25%
The arbitration board will award a percentage amount for each of the three years that lies on the range between the two parties submitted figures guided by the information supporting their numbers (the OMA’s justifications for its figures in its submission look to my eyes to be considerably stronger).
2) Continuity of Care Accountability Measure with Financial Consequences – the methodology of the measure has been agreed by the parties. But the question of whether there will be financial consequences and if so, the trigger threshold and financial magnitude, have not.
– OMA submission: no financial consequence but if so, trigger threshold should occur only if continuity falls below 70% and penalty should be a 10% reduction in base rate
– MOH submission: Trigger threshold is falling below 80% continuity and penalty should be 20% reduction in base rate
The arbitration board must first decide whether there should be a financial consequence and if so, when it should be implemented. For example, it could say that physicians need several quarterly reports to allow them to adapt their practices before the financial penalties start. With respect to the threshold, the arbitration board will likely choose a figure in the 70-80% range, though it is free to choose outside that range and here to, it could make a setting that changes over the three remaining years of the agreement. Same goes with the size of the base rate penalty, which we can assume will be in the 10-20% range if a penalty forms part of the new PSA.
** Note – Continuity of Care and any penalty is assessed at the level of each individual physician’s practice, NOT at the level of the FHO.
3) Increase to FHG premium
– OMA submission: Increase from the current 10% to 20%
– MOH submission: No change
The arbitration board may choose to keep the FHG premium the same, or increase it by any amount it wishes. Including raising it by more than 20%.
4) $5 per patient visit overhead fee for community practices (up to 40 visits per day; excludes hospital, contract and FHO/FHO+ services)
– OMA submission: Newly proposed by OMA
– MOH: No response
The arbitration board will have to decide whether to introduce this fee at all and then at what dollar rate to set the fee. Note that this fee applies to community specialist practices as well as to non-FHO family medicine practices.
The bottom line:
There is a wide range of possible financial outcomes of the arbitration board award. That’s why trying to forecast how it will affect you, or plan adaptations, will likely not be a very good use of your time at the moment.
I also think that the past week has demonstrated, yet again, the OMA’s poor member communication skills: it was irresponsible of them to publish scenarios and calculators that neither acknowledge nor take into account the possible continuity of care financial penalties. My recommendation is to generally ignore their messages until the arbitration board issues its decision.