Disclosure: I have a business relationship with Medicte, a firm that provides high quality medical tourism services for Canadians. They provided me with some information for this blog. If you are on a prohibitively long waiting list for medical or surgical services, and are willing to consider travelling out of country to have treatment, contact Dr. Abdullah Erdogan at: medical.developer@mestassistance.com
I’ve written previously about Health Data Systems and what a poor job Ontario (and indeed all of Canada) does at using information technology (IT) to help with health care. Let’s look at country that does things the right way, Turkiye (formerly Turkey). I appreciate this choice may come as a surprise to many, but Turkiye has a very modern, highly efficient health care system, and had to go through their own period of transformation from a fragmented system to a more integrated one.
The long version of how Turkiye evolved their health systems can be found here. The short version is that in 2003, the Turkish government came up with the political will to introduce the Health Transformation Program. Over the next ten years this act, and unyielding political will, transformed the Turkish health care into a fully integrated system. In many ways, it’s a model for what Canada needs to do.
I had the honour of being invited to do a talk for the Canadian Turkish Business Council on the Canadian health system (along with my smarter and more esteemed colleagues Drs. Nadia Alam and Silvy Mathew). In preparation, I studied up on how Turkiye handles health data (with the help of Medicte). I cannot tell you how impressed I was with their system.



In Turkiye, the federal government has mandated that all hospitals in Turkiye use the Hospital Information Management System (HIMS). Now to be clear, different hospitals in Turkiye still use some different modules of software, but they are all compatible with HIMS. The data for all citizens of Turkiye is then backed up securely.
Then, every citizen of Turkiye is offered a patient portal called e-Nabiz.

What does this portal allow patients in Turkiye to do? According to Medicte:
“When people enter their E-Nabız profile, they can make appointments at all public hospitals and access the records of these appointments. They can review all of their examination, diagnosis and treatment data in the health facilities they visit and access the details of all the tests performed during this process. This includes all data related to the process, such as all laboratory tests and radiology images with their reports, prescriptions, diagnoses and drug usage details.”
Further more, the app can be used to allow other health care providers access to patients health information (with consent). Let’s say a resident of Istanbul happens to travel to Antalya (a truly lovely tourist destination about an 8 hour drive away). If that person gets ill, they can use the E-Nabiz portal to allow doctors in Antalya to see their previous health information to help guide their care. Not only that, information about their visit in Antalya will automatically be available to their family doctor in Istanbul, including lab work, diagnosis, and prescriptions. I can’t even get health information on patients of mine that go to a walk in clinic in Barrie, and that’s only 30 minutes away from my office.
Not only does this system allow for much better communication between health care professionals of all kinds (physicians, nurses, pharmacists, home care and so on), but having knowledge of a patient’s previous health history significantly reduces duplication of tests. And leads to more optimal outcomes.
For people who are not citizens of Turkiye, but go there for medical tourism (Turkiye is one of the top medical tourist destinations in the world), their travel companies can offer them similar access to their health care records. For example, Medicte will soon offer the MestCard app via its parent company MestGroup.
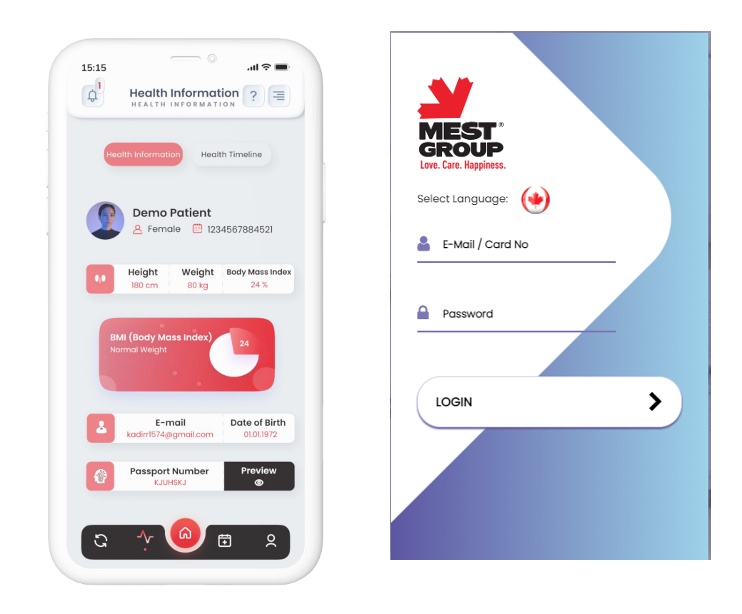
Essentially, a patient of mine, who choses not to wait the 13 months that they currently have to wait for a hip replacement in my area, could go to Turkiye next month, get their hip replaced AND have much better access to all their health records than a patient of mine who got that done in Canada. (And yes, all of these apps/software/portals are compliant with recent security standards).
But that’s not all, this tight integration of IT allows for other benefits. For example, Health Systems Consultant Matthew Lister, who spoke at the same event, informed how this allowed hospitals across Turkiye to manage their supply issues. If one hospital was short on something (tubing, a drug, IV fluid or so on), it can immediately check the inventory of nearby hospitals and request a transfer. No phone calls, no double checking. It’s all online, backed up, and available for hospital management to see. He also emphasized that this has been the case in Turkiye since at least 2011!

In Canada, given the disastrous current state of our health care system, there have been calls for system transformation from multiple sources. Whether from what are viewed as conservative organizations like the Fraser Institute and Postmedia News, or progressive organizations like Canadian Doctors for Medicare and the Torstar Media group, everyone from all sides of the political spectrum agrees that health care is need of a fix.
Here’s thought. Rather than start from scratch, let’s look at countries like Turkiye, that have taken their own fragmented health care systems, unified them and leapfrogged Canada to develop a much more efficient health system. Then just do what they did.
The benefits to the citizens of Canada would be enormous.
Post Script: While it’s true that Turkiye has a modern, high functioning health system, even such a system can be overwhelmed by a disaster like the recent Earthquake that has claimed at least 50,000 lives. To help the victims of the earthquake in both Turkiye and Syria, I encourage you to donate to the IDRF Earthquake Relief Fund.