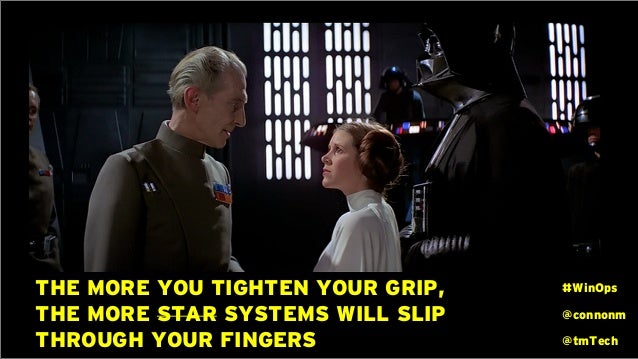
Canadians are currently dealing with the dizzying spectacle of Donald Trump’s tariffs against our country. On again? Off again? Delayed? Doubling? I’ve personally gotten seasick trying to keep up with whatever tangerine Palpatine is thinking.

However Canada’s response to this (and the nonsense about us becoming the 51st state) has frankly been quite lacking. Yes, it’s great to see Canadians being able to fly the flag with pride, especially after the miserable co-opting of the Canadian flag by the freedom convoy types, who likely themselves were Donald Trump supporters. (How’s that working out for you guys now?) Yes #elbowsupCanada is a wonderful approach to take and a great mantra going forward, particularly with how intertwined hockey is with our nation. (Quick reminder: Not only do we win Olympics, we win Four Nations Cups as well).



BUT, for all the outcropping of (absolutely warranted) national pride – our governments – outside of launching retaliatory tariffs, haven’t done anything to fix the systemic problems in our economy. For example, getting rid of domestic trade barriers and having free trade between provinces would provide a boost of up to $200 billion dollars to our economy, but seemingly no action on this yet.
Even more importantly and what’s long overdue, is an absolutely necessary look at the bureaucracy and impediments that many businesses face in trying to contribute to our economy. Let me talk about a personal experience (and no disrespect intended to the good people on staff in my township).
About 10 years ago, our community had clearly outgrown the medical centre. Some poor sap was put in charge of expanding it. (Guess who.) I had to deal a myriad of problems of putting an addition on our medical centre. Here’s a couple of examples of what I dealt with.
As per policy, the township requested that we provide an engineered site plan. The reason for this was to assess water drainage requirements. While on the surface this makes sense, all the engineered site plan was going to tell us what size of culvert to put on our property for water drainage. The estimate for the site plan was about $15,000.

However, it turns out there were only two sizes of commercial culverts for our project. A big one and a small one. The big one cost $500 more than the small one. Being well-versed in the obstinacy of Ontario Health’s bureaucrats, but somewhat naive in the inflexibility of municipal bureaucrats, I offered to simply put in the bigger culvert right from the start in exchange for waving the engineered site plan.
Those discussions went as well as my less naive readers will expect. The site plan wound up costing $17,000, and it told us that we had to put in the big culvert.
Want more? The township requested a $250,000 letter of credit or certified cheque prior to approving the expansion of the building. My initial reaction was somewhat negative to this request, but upon reflecting, I did realize that it made sense. The request was put in place in case a builder started a project, ran out of money before they finished the project, and left a hole in the ground. The money would then be used to pay to clean up the mess they made.
I still grumbled about the fact that the township was making long term doctors who were clearly invested in the community do this, but I have to concede that it was fair.
The bank informed me there’s some complex fee formula for a letter of credit – and it would have cost $5,000. I asked them for a certified cheque, and it turns out banks don’t do that anymore. However, they were willing to issue a bank draft and the fee for that was $50. Obviously, I got the bank draft instead.
When I went to the planning office however, I was told this was unsuitable. The contract we signed specifically asked for a Letter of Credit or Certified Cheque and I had presented neither. Therefore we had not met the terms of our contract and the project would come to a halt. The staff person did offer to take this to the planning committee, and six weeks later they decided this was ok.
Is this me just griping? Nope – in fact his is happening all through health care and businesses in Canada. I recently spoke to the owner of a Nursing Home. His home had been approved on a “fast track” for a new build based on the dire shortage of nursing home beds in Ontario. I asked when the facility would be built and he just laughed. Apparently “fast track” means that there will “only” be 30 months of paper work (!) before the shovels go in the ground and he hopes it will be completed in 5-6 years!! I’m guessing this “fast track” must be on Toronto’s Eglinton LRT line….

Want more? Just look at the saga of my local hospital, the Collingwood General and Marine. We’ve known for almost two decades that it’s far too small for the community. Heck the community has been asking for a new hospital since the early 2010s and finally got approval on phase 1 (of 5) in 2016. And 9 years later (!) we are at phase 3. The “hope” is that the new building will open its doors in 2032 – 16 YEARS after it was absolutely clear a new hospital was needed immediately.
This problem is not restricted to the health care sector of course. The Financial Post had a piece in 2019 (!) about how these rules are affecting multiple industries. Not only are we not building critical infrastructure in a timely manner because of an inability to cut the bureaucratic bloat, but it’s stifling private businesses as well. The Canadian Chamber of Commerce pointed out that the “ease” of doing business has gone from fourth in the world in 2006 to 53rd now, and this impedes economic growth and investment.
New Prime Minister Mark Carney is off to Europe this week to build trade and strengthen relations. Nothing wrong with that, we need reliable trade partners in the future. BUT, we face an unhinged, hyper volatile situation with our neighbours to the south RIGHT NOW. It seems to me there is no better time than now to drop intra Provincial trade Barriers and right size the bureaucracy allowing for businesses to grow and thrive more easily in Canada. As for health care, the right time was 10 years ago.