OMA Elections will soon be upon us. This year the possibility of significant change to the organization exists as half of all physician Board Director positions are up for grabs. A review of the OMAs election page shows that there are 58 (!) candidates running for 4 Board positions.
My three loyal readers know that I have long felt that the first and foremost responsibility of the OMA is member advocacy. Many have heard me say time and time again that you cannot have a high functioning health care system without happy, healthy and engaged physicians. The OMA needs to consistently and effectively promote physicians.
Unfortunately the government of the day continues to disrespect physicians by forcing us into a never ending arbitration process. It also, despite the correct warnings of the OMA, continues to expand the scope of practice of non-physicians. I therefore wanted to see which of the Board candidates would be willing to take a more aggressive approach to this issue. So on a bunch of Social Media forums, I posted a request for all Board Candidates to sign a pledge if elected.
What exactly was this “pledge”? Was it a demand to remove the compulsory dues that all physicians have to pay to the OMA? Was it to split the OMA into two organizations- one for specialists and one for family doctors like they have in Quebec? A demand to fire certain staff?
Nope. It was a pledge to get data on how much allied health care providers (in this case NPs) cost the health care system when they try to do the work of family physicians. See below:
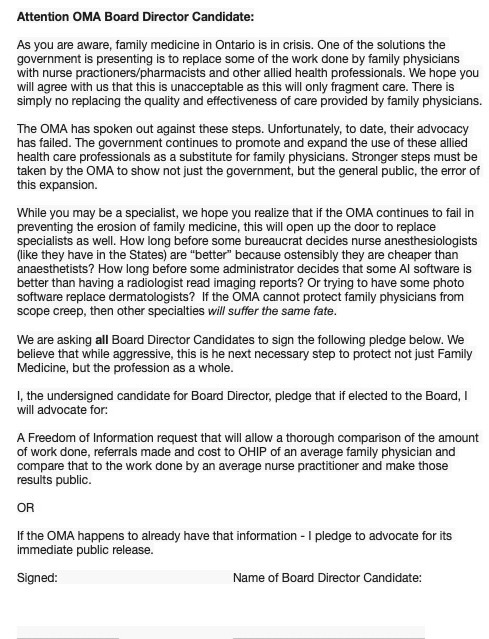
Now, did I think the culture of the OMA, that has been put in place by and is overseen by the current Board, would be happy with this? Of course not. Despite what my kids tell me, I’m not that out of touch. I expected some sort of push back suggesting this was (in their view) inappropriate.
But I confess I was taken aback by not only the factual errors in their response, but what quite frankly can only reasonably be perceived to be a veiled threat to myself and Board candidates. Here’s a copy of what I got:

The first factual error is to conflate the governance transformation (which I supported, and still do) with the elections process. The governance transformation was about reducing the size of the Board, and making it electable by and therefore responsible to the membership as a whole. This is opposed to the mishmash of ways people got on the Board before. It was also about sunsetting OMA Council (which had long served it’s purpose) and putting in a better, more co-operative General Assembly system, along with a Priorities and Leadership group to advance the needs of the members.
I did, and continue to support all of that (trust me, the old system was much worse). BUT – that is completely separate from the elections process itself. The intense over regulation of what candidates can and cannot say or how they can act during elections is NOT governance transformation, it’s micromanagement.
The second error is to suggest that it is because of my previous role at the OMA that I am “viewed as a leader”. Apart from the obvious fact that I have a bunch of detractors, the blunt reality is that there are a whole lot of ex-OMA Presidents out there who would not have influence because of the title itself. They have influence because of who they are/what they advocate for/actions they take outside of any past title.
The email to OMA Board Director candidates was almost as bad:

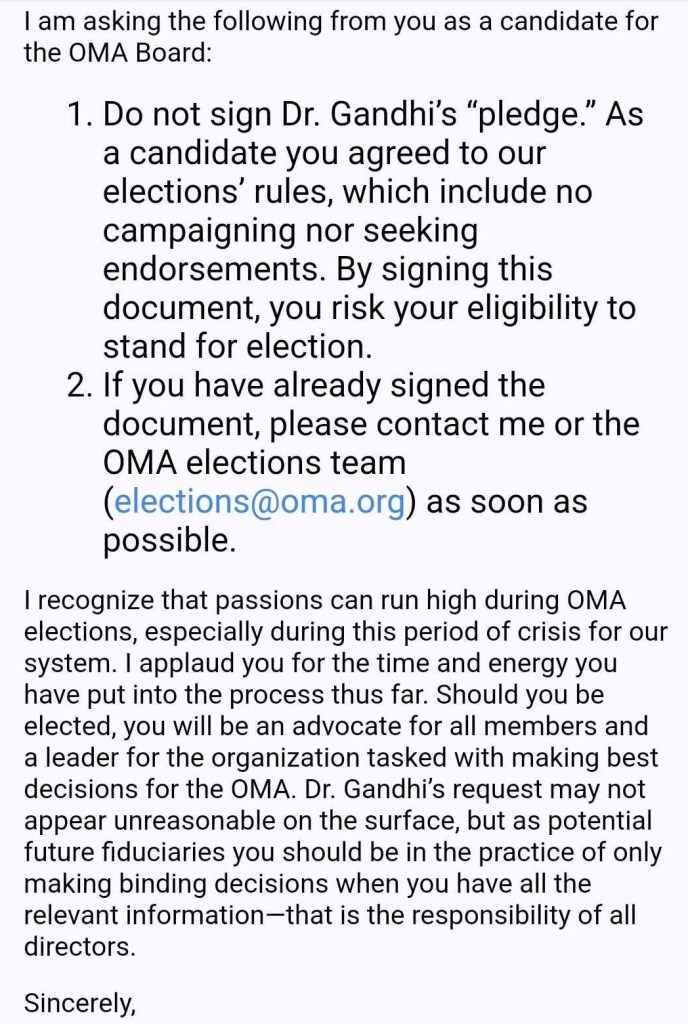
The underlying message is quite clear. Sure you can run for Board Director. BUT, if in OUR opinion, you “campaign”, or take a position WE don’t like, or speak out of turn – WE disqualify you. Intentionally or not, it creates the impression that the organization only wants a certain kind of Board Director. Not a strong independent type who can think on their own, and, dare I say it, take a bold stance that perhaps requires come chutzpah (like signing the pledge would!) But rather a benign, meek, Board Director – who will simply rubber stamp what’s been presented to them.
Unacceptably, in my view, is the more subtle threat of damaging our careers. The comment that this is”not in keeping with OMA’s code of conduct and civility”can really only be viewed as a veiled threat. Charging someone under a code of conduct violation has the potential to be extremely damaging. Many physicians, when they apply for new positions have to answer questions like “are they now under investigation” for such and such, even if there has not been a ruling yet. Being charged with this would force them to answer yes and potentially damage career options.
To be clear, I actually support the code of conduct and civility. I saw in the aftermath of the miserable 2017 tPSA debacle some incredibly unprofessional comments made towards the OMA staff (and others). I also am aware of many instances since where staff have been verbally abused by members and that is completely unacceptable. The staff are a very hard working bunch – who follow the direction and the culture the Board puts in place. It’s the Board that should be – respectfully – held into account.
But to tell a potential Board Director candidate (and me) that stating an opinion that might be viewed as controversial and advocating for that as part of an election process might see them charged?? Especially when there was absolutely no foul/derogatory/demeaning language used in the posts? Sorry but that simply comes across as attempting to censor a view point that you don’t happen to like. And that’s just wrong. Worse, it gives credence to the many critics of the policy who feared it would be used to suppress discussion.
Members deserve a strong, independent thinking and bold OMA Board. An elections process that goes to these extremes to prevent candidates from taking a stand on issues, advertising to members their skills (or lack thereof!) and their philosophy does not serve the membership at all. It will only disenfranchise them and lead to more voter apathy. About the only thing members can do at this point is NOT vote for any incumbents for Board Director and hope that will trigger some changes to this process.
As for me, I will try to get through the elections material – and pick candidates who I think will work to change the organization for the better. I will let you know my thoughts in a later blog.