I’ve written about the horrific treatment that Dr. Elaine Ma has been subjected to by the bureaucrats at Ontario Health before. The situation is so ridiculous that it could be a story presented at the Theatre of the Absurd.
What happened?
Dr. Ma is a family physician from the Kingston area. During the Covid pandemic she realizes the need to immunize as many people as possible to protect the community. She organizes a number of outdoor mass vaccination clinics, which resulted in Kingston being one of the most heavily vaccinated areas of the province. For her efforts, she wins the very well deserved the praise of many, and an award from the Ontario College of Family Physicians.
There are two billing codes for providing Covid vaccinations. One for physicians who work in a vaccination clinic that someone else set up (e.g. public health). Another for those who set up the clinics themselves, and paid for staff/heating for outdoors/tents/internet etc. Since she paid for all of that, Dr. Ma bills the second code.

Fast forward a couple of years and the callous and unthinking bureaucrats at OHIP decide that she has billed the wrong code and demand she pay back $600,000. I won’t restate all the steps she went through to fight this. I will state that the reasons for them wanting the money paid back varied between the clinic being outdoors instead of indoors, medical students being involved and so on. But eventually the case winds up at Divisional Court.
On Dec 16, the court handed down a ruling supporting Dr. Ma. What I had failed to realize before is that the Ontario Health bureaucrats main argument appears to be that there were no extenuating circumstances during the time of the Vaccine Clinics that Dr. Ma set up. Yes, you read that correctly. The whole country was in the midst of a (hopefully) once in a lifetime pandemic. Canada was effectively shut down for business. People were not allowed to visit loved ones in hospital or nursing homes. Travel had ground to a halt. But, in the minds of the soulless and spiteful bureaucrats, none of this constituted “extenuating circumstances”.
Thankfully, Divisional Court Justices Matheson, Varpio and O’Brien were having none of this nonsense. They clearly stated the decision by bureaucrats that there were no extenuating circumstances was “unreasonable.” (I would have, and will, call that decision much worse things). The Justices pointed out the obvious. There was clearly a public health crisis at the time, and that many leaders, including politicians were calling on physicians to get the vaccinations done.
More importantly they stated something the OMA’s legal team really needs to take a deep dive into:
…”that the wording of section 17.5 does not limit relief to unpaid claims; it only requires the presence of extenuating circumstances. Since OHIP typically pays claims first and reviews them later, a restriction on unpaid claims would effectively nullify the provision. The court called this interpretation unreasonable.”
Currently OHIP pays physicians whenever they bill. Later, OHIP decides if it was reasonable or not, and if OHIP feels the situation is unreasonable, they demand the money back. The justices seem to be saying this process is not fair. Which has implications far beyond this one case. Obviously, this would not apply to clear cut cases of fraud. It is a much much needed kick to the slow, incompetent, and spiteful OHIP review process. I can’t possibly understand the potential future implications for this – but I suspect there will be many.
Finally, the justices let their displeasure be known by ordering OHIP to pay Dr. Ma $10,000 in court costs. This strongly suggests to me that they were peeved at the OHIP bureaucrats for taking it this far, and really didn’t think it should have gone there.
How is this hurting health care now?
Ontario is currently seeing an unprecedented surge in flu cases. Flu season has come early. The current variant appears to be extremely strong. It is circulating at “sky high” levels among young people. Three children (at least) have died. Hospitals have declared outbreaks and wards are closed. Visitation has stopped.
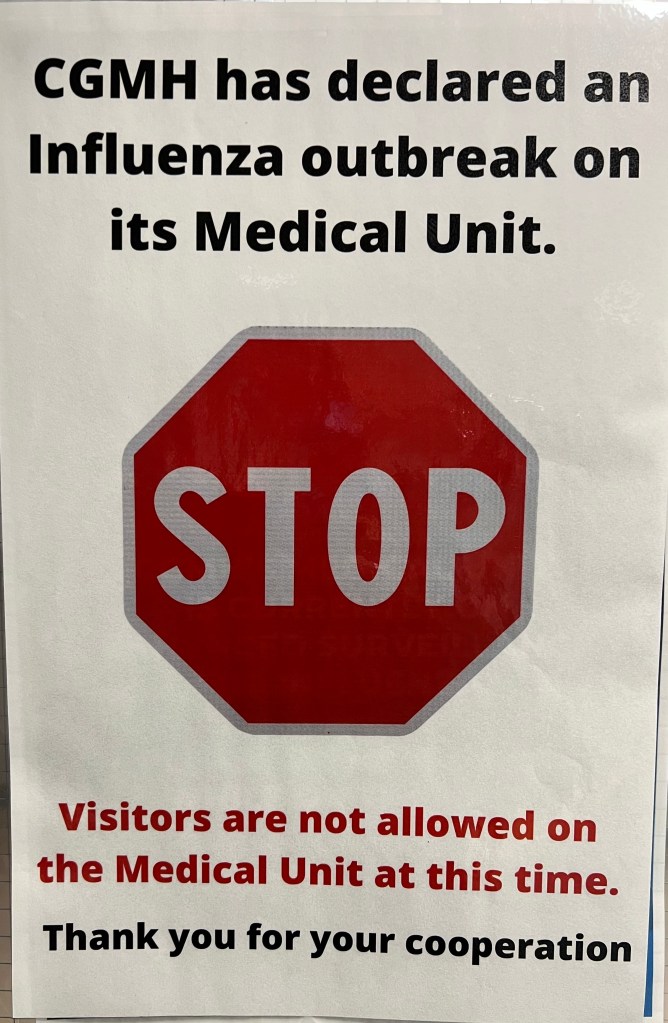
You know what would really help? If only some people would come up with some innovative ways of getting their communities vaccinated against the flu. Yes this year’s flu shot is a bit of mismatch for the current strain, but it still provides some protection and keeps you from getting really ill.
Or how about an innovative idea for where to safely look after patients like was done during the Covid crisis. My friend Dr. Bryan Recoskie set up a unique 18 bed ward in our local Legion, to look after non-covid patients while the hospital wards were shut with covid positive patients.

And yet, I don’t see any of that happening right now. Don’t get me wrong, doctors continue to go to work. We continue to care for the sick and continue to comfort those in need. We continue to do our best in these trying circumstances.
But I can’t find any evidence (please correct me if I’m wrong) – of where people are doing unique out of the box things to try and mitigate the currently unfolding nightmare. Given the potential exists that IF you try something unique, you may wind up undergoing two years of pure hell by bitter, ruthless and depraved bureaucrats – can you blame people for not trying?
To quote a good friend of mine, “The damage has been done. Nobody is going to stick their necks out now.”
What should happen (but won’t):
First, under no circumstances should OHIP appeal the decision from Divisional Court. The mercilessly inhumane bureaucrats need back down. Second, Health Minister Sylvia Jones needs to do what she should have done a year ago – and direct the bureaucrats not to seek any recovery at all from Dr. Ma. It’s just the right and decent thing to do.
Finally, it would really help if Minister Jones issued a formal apology to Dr. Ma for how she has been treated by the bureaucrats. It’s not just the OHIP bureaucrats. Jones’ own communications director, Hannah Jensen claimed Dr. Ma had “pocketed the funds“, a statement that clearly suggested malfeasance.
Do that, and maybe, just maybe, physicians would once again feel comfortable coming up with out of the box solutions for crises that are occurring.
Maybe.