The Honourable François Legault, M.L.A.
Premier of the Province of Quebec
Édifice Honoré-Mercier, 3e étage
835, boul. René-Lévesque Est
Quebec QC G1A 1B4
Dear Premier Legault,
You probably don’t know who I am, and are wondering what propelled me to write an open letter to you. I decided to write to you after doing a radio interview with Greg Brady on his show Toronto Today. During the interview, Greg asked me to comment on the strife between you and the physicians in your province. He brought up the fact that in the past couple of weeks, 263 physicians from Quebec have applied for a licence to practice medicine in Ontario.
Now, I certainly don’t pretend to be an expert in how the health system functions in Quebec. Nor would I assume to know all of the intricacies of Bill 2, the legislation that you’ve introduced that has your physicians so angry. And no, I’ll say right off the bat, I don’t know what negotiations between you and the representative bodies of physicians in Quebec (FMSQ and FMOQ)have been like.
But I will tell you that my very first blog ever (in the Huffington Post) was an open letter to Ontario’s then health minister, Dr. Eric Hoskins. I wrote that blog because his government was talking unilateral actions against physicians (sound familiar?) In it, I warned Dr. Hoskins that acting in a unilateral manner would result in chaos for our health system:
“We cannot return to a system where there are three million or more people without a family doctor, or wait times to see specialists (already too long in my area) get prohibitively longer.”
I also warned of the political consequences of proceeding with unilateral actions and how this would hurt Liberals in the 2018 election. You perhaps know they were absolutely decimated in that election. While its true a large part of that defeat was because the feckless Premier Kathleen Wynne was so widely disliked, I maintain to this day the Liberals could at least have maintained official party status had they not botched health care so badly.
The reason I could make those statements in my blog with such absolute certainty, and have them proven right in the end was not because of any prescience on my part. It’s because I followed the advice of Santayana:

Look, I understand that some of the specifics of the policies and legislation that you are bringing in are different from what Dr. Hoskins tried to do. But at the end of the day, it amounts to you as a government saying that you know how to run healthcare. You don’t need advice or co-operation from doctors. You’re going to impose the changes you want.
I’d encourage you to go back and read the letter I wrote to Dr. Hoskins. I pointed out to him that he was repeating the mistakes (unilateral actions) of the Bob Rae NDP government in the 1990s. They destroyed health care by those actions and were wiped out in the 1995 election, never to see power again.
Take a look at the Jason Kenney PC government of 2019. The went to war with Alberta Medical Association in 2020. The only way they were able to salvage a victory in the next election after that, was to dump their leader, Jason Kenney. (It’s true unhappiness with how he handled the Covid pandemic played a role – but again, the point is there was no saving grace for him – if he had kept health care functioning…..)
Want more? Look at the actions of the Gordon Campbell British Columbia government. Between 2001-2002 they unilaterally tore up an arbitration agreement between the BC government and their doctors. Years of discord including a Charter Challenge (that the BC Government eventually lost), political strife, a strike vote by physicians and a vastly reduced majority followed. Eventually, given a failing health system caused by their own arrogance, the BC government had to come to an agreement with their doctors in 2002, and again in 2006 that restored binding arbitration and was viewed as extremely generous at the time.
As I pointed out to Dr. Hoskins the message is simple. Any government that takes on unilateral action will run the risk of losing doctors from that province. When that happens, the healthcare system suffers. When that happens patients suffer, wait times go up, care deteriorates. When that happens, people don’t blame the doctors, they blame the politicians.
In short, a government that imposes unilateral actions on physicians not only hurts the patients of their province, they always pays a political price. They always have to pay more in the long run than if they just worked fairly with their physicians in the first place.
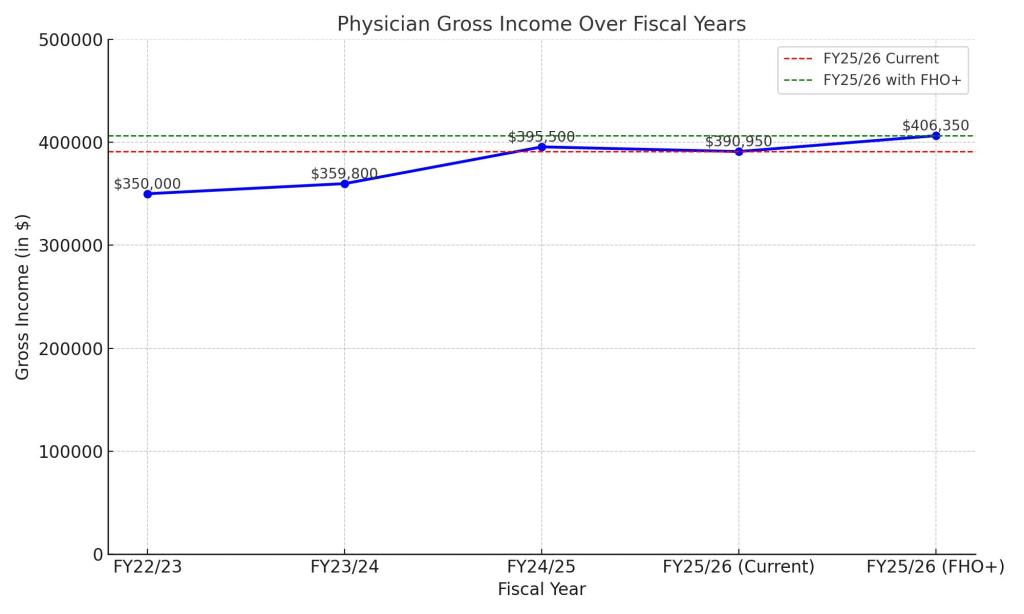
Look, I don’t particularly care about you or your government. I could not care less whether you win or lose your next election. But I happen to care a lot about my physician colleagues and I know that they are very very angry (and rightfully so). I also care about the residents of Quebec, and I know that they are going to suffer a lot because of your actions. As of now, 28% of your population does not have a family doctor. Can you imagine what will happen if 263 leave? And do you really think any doctor with half a brain will actually come to Quebec when your government behaves like this?
Trust me on this one, if you don’t immediately reverse course, and start to work with your doctors – the harm done to your health system and the people you are supposed to serve will be enormous.
And if you don’t believe me – go read that quote from Santayana again.
Yours truly,
An Old Country Doctor